What is Alcoholic Hepatitis
Alcoholic hepatitis Definition
Definition
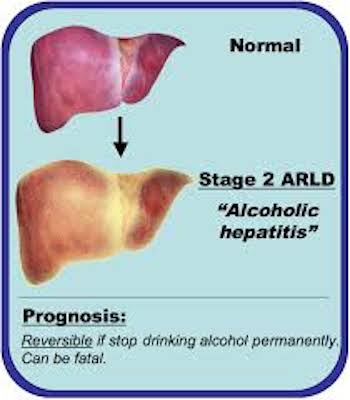
Alcoholic hepatitis describes liver inflammation caused by drinking alcohol.
Though alcoholic hepatitis is most likely to occur in people who drink heavily over many years, the relationship between drinking and alcoholic hepatitis is complex. Not all heavy drinkers develop alcoholic hepatitis, and the disease can occur in people who drink only moderately.
If you're diagnosed with alcoholic hepatitis, you must stop drinking alcohol. People who continue to drink alcohol face a high risk of serious liver damage and death.
Symptoms
Yellowing of the skin and whites of the eyes (jaundice) and increasing girth (due to fluid accumulation) are the most common signs of alcoholic hepatitis that lead people to seek medical care.
People may also complain of:
Loss of appetite
Nausea and vomiting
Abdominal pain and tenderness
Weight loss
Just about everyone who has alcoholic hepatitis is malnourished. Drinking large amounts of alcohol suppresses the appetite, and heavy drinkers get most of their calories in the form of alcohol.
Signs and symptoms of severe alcoholic hepatitis include:
Retaining large amounts of fluid in your abdominal cavity (ascites)
Confusion and behavior changes due to brain damage from buildup of toxins (encephalopathy)
Kidney and liver failure
When to see a doctor
Alcoholic hepatitis is a serious disease. As many as 35 percent of heavy drinkers develop alcoholic hepatitis. And more than a third of them die within six months after signs and symptoms begin to appear.
See your doctor if you have any signs or symptoms of alcoholic hepatitis or other signs and symptoms that worry you. If you ever feel as though you can't control your drinking or feel that you'd like help in cutting back on your drinking, see your doctor.
Causes
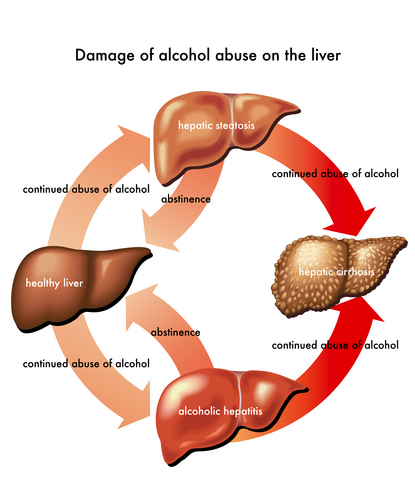
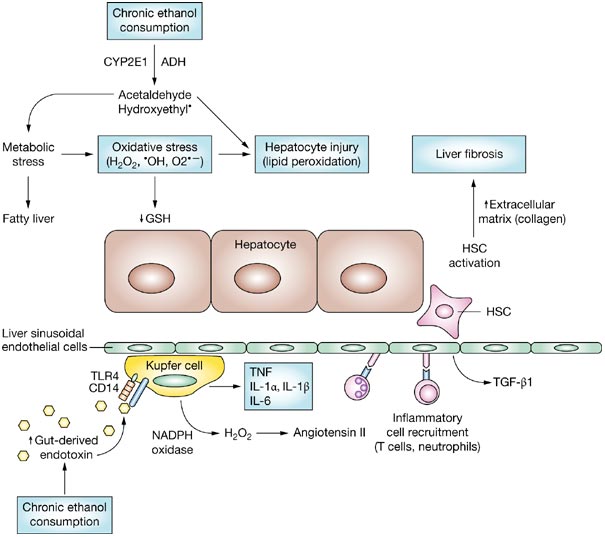
Alcoholic hepatitis occurs when the liver is damaged by the alcohol you drink. Just how alcohol damages the liver -— and why it does so only in a minority of heavy drinkers — isn't clear. What is known is that the process of breaking down ethanol — the alcohol in beer, wine and liquor — produces highly toxic chemicals, such as acetaldehyde. These chemicals trigger inflammation that destroys liver cells. Over time, web-like scars and small knots of tissue replace healthy liver tissue, interfering with the liver's ability to function. This irreversible scarring, called cirrhosis, is the final stage of alcoholic liver disease.
Risk increases with time, amount consumed
Heavy alcohol use can lead to liver disease, and the risk increases with the length of time and amount of alcohol you drink. But because many people who drink heavily or binge drink never develop alcoholic hepatitis or cirrhosis, it's likely that factors other than alcohol play a role. These include:
Other types of hepatitis. Long-term alcohol abuse worsens the liver damage caused by other types of hepatitis, especially hepatitis C. If you have hepatitis C and also drink — even moderately — you're more likely to develop cirrhosis than if you don't drink.
Malnutrition. Many people who drink heavily are malnourished, either because they eat poorly or because alcohol and its toxic byproducts prevent the body from properly absorbing and breaking down nutrients, especially protein, certain vitamins and fats. In both cases, the lack of nutrients contributes to liver cell damage.
Obesity.
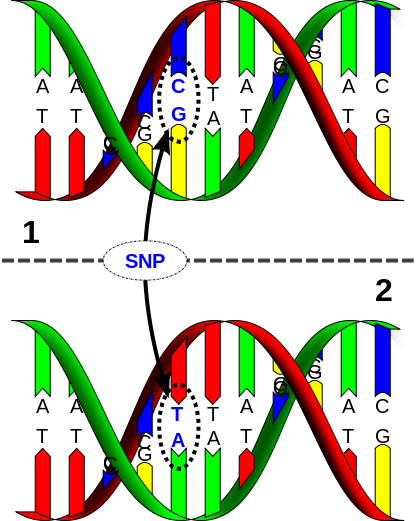
Genetic factors. Having mutations in certain genes that affect alcohol metabolism may increase your risk of alcoholic liver disease as well as of alcohol-associated cancers and other complications of heavy drinking. The exact genetic associations have not yet been identified.
Risk factors
Major risk factors for alcoholic hepatitis comprise:
Alcohol use. The amount of alcohol consumed is the most important risk factor for alcoholic liver disease. One study found that the risk of cirrhosis of the liver increased with daily ingestion of more than 2 to 2.8 ounces (60 to 80 grams) of alcohol over 10 years for men and 0.7 ounces (20 grams) for women. Yet still, only about 35 percent of heavy long-term drinkers develop alcoholic hepatitis.
Your sex. Women have a higher risk of developing alcoholic hepatitis than men do. This disparity may result from differences in the way alcohol is processed by women.
Genetic factors. A number of genetic mutations have been identified that affect the way alcohol is broken down in the body. Having one or more of these mutations may increase the risk of alcoholic hepatitis.
Other factors which may increase your risk include:
Type of beverage (beer or spirits are riskier than wine)
Binge drinking
Obesity — alcohol and obesity may have a synergistic effect on the liver; that is, their combined effect is worse than the effect of either of them alone
African-American or Hispanic
Complications
Complications of alcoholic hepatitis include:
Increased blood pressure in the portal vein.
Blood from your intestine, spleen and pancreas enters your liver through a large blood vessel called the portal vein. If scar tissue slows normal circulation through the liver, this blood backs up, leading to increased pressure within the vein (portal hypertension).
Enlarged veins (varices).
When circulation through the portal vein is blocked, blood may back up into other blood vessels in the stomach and esophagus. These blood vessels are thin walled, and because they're filled with more blood than they're meant to carry, they're likely to bleed. Massive bleeding in the upper stomach or esophagus from these blood vessels is a life-threatening emergency that requires immediate medical care.
Fluid retention.
Alcoholic hepatitis can cause large amounts of fluid to accumulate in your abdominal cavity (ascites). The fluid may become infected and require treatment with antibiotics. Although not life-threatening in itself, ascites is usually a sign of advanced alcoholic hepatitis or cirrhosis.
Jaundice. This occurs when your liver isn't able to remove bilirubin — the residue of old red blood cells — from your blood. Bilirubin builds up and is deposited in your skin and the whites of your eyes, causing a yellow color.
Hepatic encephalopathy. A liver damaged by alcoholic hepatitis has trouble removing toxins from your body — normally one of the liver's key tasks. The buildup of toxins can damage your brain, leading to changes in your mental state, behavior and personality (hepatic encephalopathy). Signs and symptoms of hepatic encephalopathy include forgetfulness, confusion and mood changes, and in the most severe cases, coma.
Scarred liver (cirrhosis). Over time, the liver inflammation that occurs in alcoholic hepatitis can cause irreversible scarring of the liver (cirrhosis). Cirrhosis frequently leads to liver failure, which occurs when the damaged liver is no longer able to adequately function.
Kidney failure.
Preparing for your appointment
Start by seeing your family doctor or a general practitioner. If your doctor thinks you have a liver problem, such as alcoholic hepatitis, you'll likely be referred to a digestive disease specialist (gastroenterologist).
Here's some information to help you get ready for your appointment, and what to expect from your doctor.
What you can do
Be aware of any pre-appointment restrictions. Ask if there's anything you need to do in advance, such as restrict your diet.
Write down any symptoms you're experiencing, including any that may seem unrelated to the reason for which you scheduled the appointment.
Write down key personal information, including any major stresses or recent life changes. Let your doctor know how much alcohol you regularly consume. It's a good idea to track your alcohol consumption for a few days by writing it down, because people tend to underestimate the amount they've consumed.
Make a list of all medications, as well as any vitamins or supplements, that you're taking.
Take a family member or friend along to help you remember everything that was said.
Write down questions to ask your doctor.
Questions to ask your doctor
For alcoholic hepatitis, some basic questions to ask your doctor include:
What's the most likely cause of my symptoms?
Are there any other possible causes for my symptoms?
What kinds of tests do I need? How should I prepare for them?
Is my condition temporary or chronic?
What treatments are available? Which one do you recommend?
Are there any alternatives to the primary approach that you're suggesting?
What resources are available to help me stop drinking? Which ones will my insurance pay for?
I have other health conditions. How can I best manage them together?
Are there any dietary restrictions that I need to follow?
Should I see a specialist? What will that cost, and will my insurance cover it?
Are there any brochures or other printed material that I can take with me? What websites do you recommend?
Don't hesitate to ask questions anytime you don't understand something.
What to expect from your doctor
Be ready to answer questions that your doctor is likely to ask:
When did you first begin experiencing symptoms?
Have your symptoms been continuous or occasional?
How severe are your symptoms?
What, if anything, seems to improve your symptoms?
What, if anything, appears to worsen your symptoms?
How often do you drink alcohol, and how many drinks do you usually consume?
Have you ever had hepatitis or yellowing of the skin before?
Do you use any other recreational drugs?
Are your family members or friends concerned about your drinking?
Do you get angry or anxious when the subject of your drinking is discussed?
Do you feel guilty about drinking?
Do you drink in the morning — do you need an eye-opener?
What you can do in the meantime
Stop drinking alcohol if you think it may be causing your health problems. If you believe you're dependent on alcohol, your doctor can recommend treatment options. However, if you need help to stop drinking while you're waiting to see your doctor, Alcoholics Anonymous or counseling may be helpful.
Tests and diagnosis
Identifying alcoholic liver disease depends on two main things:
Evidence of excessive alcohol consumption
Evidence of liver disease
Alcohol consumption
Your doctor will want to know about your history of alcohol consumption. It is important to be honest in describing your drinking habits. Your doctor may ask to interview family members about your drinking. Many people will have signs of chronic alcoholism, such as skin lesions known as spider nevi.
Liver disease
Your doctor will likely order the following tests to look for liver disease:
Liver function tests (including international normalized ratio, total bilirubin, and albumin)
Complete blood cell count
An ultrasound, CT or MRI scan of the liver
Blood tests to exclude other causes of liver disease
Nov. 03, 2012
Treatments and drugs
Stop drinking alcohol
If you've been diagnosed with alcoholic hepatitis, you must stop drinking alcohol. It's the only way of possibly reversing liver damage or, in more advanced cases, preventing the disease from becoming worse. Many people who stop drinking have dramatic improvement in symptoms in just a few months.
If you continue to drink alcohol, you're likely to experience serious complications.
If you are dependent on alcohol and want to stop drinking, your doctor can recommend a therapy that's tailored for your needs. This might include medications, counseling, Alcoholics Anonymous, an outpatient treatment program or a residential inpatient stay.
Treatment for malnutrition
Your doctor may recommend a special diet to reverse nutritional deficiencies that often occur in people with alcoholic hepatitis. You may be referred to a dietitian who can help you assess your current diet and suggest changes to increase the vitamins and nutrients you are lacking.
If you have trouble eating enough to get the vitamins and nutrients your body needs, your doctor may recommend tube feeding. This may involve passing a tube down your throat and into your stomach. A special nutrient-rich liquid diet is then passed through the tube.
Medications to reduce liver inflammation
Your doctor may recommend corticosteroids drugs if you have severe alcoholic hepatitis. These drugs have shown some short-term benefit in increasing survival. Steroids have significant side effects and are not recommended if you have failing kidneys, gastrointestinal bleeding or an infection. About 40 percent of people do not respond to corticosteroids. Your doctor may also recommend pentoxifylline, especially if corticosteroids don't work for you. Some studies of pentoxifylline have shown some benefit, others have not. You might also ask about clinical trials of other therapies.
Liver transplant
For many people with severe alcoholic hepatitis, liver transplant is the only hope to avoid death. Survival rates for liver transplant for alcoholic hepatitis are similar to those for other forms of hepatitis, greater than 70 percent five-year survival.
However, most medical centers are reluctant to perform liver transplants on people with alcoholic liver disease because of the fear they will resume drinking after surgery. For most people with alcoholic hepatitis, the disease is considered a contraindication for liver transplantation in most transplant centers in the U.S.
For transplant to be an option, you would need to find a program that will consider you. You would have to meet the requirements of the program, including abstaining from alcohol for six months prior to transplant and agreeing not to resume drinking afterward.