MELD and the Waiting List for Liver Transplant
Meld Score and Transplant
Livers are donated in the spirit of altruism and are a limited national resource; thus, it is only right that donor livers be allocated in a fair manner. California Pacific Medical Center’s Liver Transplant Program adheres to national policies developed by the United Network for Organ Sharing (UNOS). UNOS has a federal contract to operate the National Organ and Procurement and Transplantation Network.
The local federally designated Organ Procurement Organization, California Transplant Donor Network (CTDN), facilitates equitable distribution of donor livers between the local liver transplant centers (Stanford, CPMC and University of California, San Francisco).
CTDN acts as a bridge between a donor hospital (a hospital with a patient who is an organ donor) and the local transplant centers. It is the policy of UNOS that all potential recipients of organ transplants must be listed on the national UNOS computer waiting list, with the priority for a donor organ determined by factors discussed below.
Donor organs that become available in the local area are offered to patients on the waiting list of one of the three local liver transplant centers. Occasionally, there is not a good match for any patient at the three centers and a donor liver is sent out of the local area; conversely, we sometimes receive livers from distant hospitals, particularly for the most ill patients.
In general, a donor is matched to a potential recipient on the basis of several factors: ABO blood type, body size, degree of medical urgency and MELD score (Model for End-Stage Liver Disease). UNOS uses a computerized point system to distribute organs in a fair manner.
Recipients are chosen primarily on the basis of medical urgency within each ABO blood group. Waiting time is only a factor when patients have the same MELD score.
In summary, the priority of an individual patient on the UNOS waiting list for a donor liver depends on the following factors:
Local versus distant (donor organs are first offered locally within the Northern California/Bay Area)
ABO type (priority is identical > compatible > incompatible ABO blood type)
Body size (the acceptable body range is determined by the transplant surgeon)
Degree of medical urgency as determined by the MELD score (highest priority given to Status 1 patients)
What is MELD? How will it be used?
The Model for End-Stage Liver Disease (MELD) system was implemented February 27, 2002 to prioritize patients waiting for a liver transplant. MELD is a numerical scale used for adult liver transplant candidates. The range is from 6 (less ill) to 40 (gravely ill). The individual score determines how urgently a patient needs a liver transplant within the next three months. The number is calculated using the most recent laboratory tests.
Lab values used in the MELD calculation:
Bilirubin, which measures how effectively the liver excretes bile;
INR (formally known as the prothrombin time), measures the liver’s ability to make blood clotting factors;
Creatinine, which measures kidney function. Impaired kidney function is often associated with severe liver disease.
Serum Sodium – a recent addition to the lab values used.
Within the MELD continuous disease severity scale, there are four levels. As the MELD score increases, and the patient moves up to a new level, a new waiting time clock starts. Waiting time is carried backwards but not forward. If a patient moves to a lower MELD score, the waiting time accumulated at the higher score remains.
When a patient moves to a higher MELD score, the waiting time at the lower level is not carried to the new level. The clock at the new level starts at 0. (Example: Patient has a MELD score of 15 and has been at level 11-18 for 100 days.
With new laboratory tests, the patient’s MELD score is 22. The patient moves to a new MELD level of 19-24. The patient’s waiting time at this new level starts at 0 days). Waiting time is only used as a tie-breaker when patients have the same MELD score.
The four MELD levels are:
greater than or equal to 25
24-19
18-11
less than or equal to 10
To determine your score, you can enter your lab values into the UNOS MELD calculator.
When should laboratory tests be done?
The frequency of laboratory tests, for those patients not in the hospital, will be determined by the patient’s medical condition, ongoing treatments, and MELD score. Your physician may recommend that labs be done more frequently than the MELD score recommendation.
The score only indicates how often labs need to be input into the UNOS database. Discuss with your physician and/or transplant coordinator how often lab tests need to be done. If you have a high MELD score and labs are not done at the frequency recommended, your MELD score will automatically be downgraded by UNOS to 6, until new lab results are received and entered into the UNOS database.
Lab Test Frequency
MELD score greater than or equal to 25; Labs needed every 7 days
MELD score 24-19; Labs needed every 30 days
MELD score 18-11; Labs needed every 90 days
MELD score less than or equal to 10; Labs needed every year
Special case exceptions
There are four Special Case Exceptions that will be assigned a higher MELD score than that assigned by the patient’s laboratory test results:
Hepatocellular Carcinoma (Liver Cancer)
Hepatopulmonary Syndrome (Abnormal changes within the lung which results from the high pressure within the liver. Results in severe shortness of breath because of the extremely low level of oxygen. Patient usually needs oxygen therapy)
Familial Amyloidosis ( Rare, chronic disease resulting in accumulation of an abnormal fibrillar scleroprotein (amyloid), which infiltrates body organs and can cause life threatening organ damage.)
Primary Oxaluria (Metabolic disorder seen in pediatric patients only).
In addition to the previously mentioned four special case exceptions, a transplant center can apply for a MELD exception for a patient whose medical urgency is not reflected by the MELD score.
Previous exceptions for ascites, spontaneous bacterial peritonitis, variceal bleeding and encephalopathy are no longer allowed unless approved by the regional review board after your team makes an appeal for special cases.
What is the average MELD score for a patient undergoing transplant?
Currently, the average MELD score for a patient undergoing a liver transplant is 20 nationally. The average MELD score for liver transplant patients in California varies from 26-33, depending on blood type.
The average waiting time for a patient to receive a liver in California, once a patient is placed on the UNOS waiting list, is 12-36 months. This waiting time may be very short for a patient with very high MELD scores and especially those with acute liver failure.
Waiting time varies according to blood type, e.g. patients with O blood type wait longer on average, and patients with B, A & AB blood type wait a shorter period of time. The severity of a patient’s liver disease and any contributing medical illnesses, such as kidney failure and/or liver cancer, may result in a patient receiving a higher MELD score.
As a patient’s MELD score increases, the priority to receive a liver transplant increases. If a patient’s condition improves, and the MELD score decreases, the priority to receive a liver transplant decreases.
Transplant physicians, nurses and social workers cannot accurately predict when a donor liver will become available for an individual patient. The availability of donors is too variable and the lists at the local transplant centers can fluctuate every day.
It is our policy not to inform patients where they are on our list, because this information does not allow us to make any accurate prediction regarding the timing of transplantation. You will be informed of your MELD score and how often your laboratory and other diagnostic tests should be done.
If you have any questions regarding the waiting list, please contact your transplant coordinator or one of the transplant physicians who will provide further information as available.
Related Posts
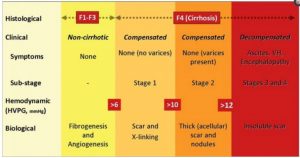
This article is a wonderful description of cirrhosis and it’s major symptoms. Everyone with cirrhosis should read this and learn from it. Craig Liver disease is the most common non–AIDS-related cause of mortality in HIV-infected patients. HIV-infected patients with chronic liver disease progress more rapidly to cirrhosis, and those with hepatitis B virus or hepatitis…
Federal Standard May Be Thwarting Some Liver Transplant Patients By EDITOR • JUN 7, 2016 Did revised federal standards make transplant centers more averse to risk and encourage them to drop sicker patients who might affect the hospitals’ patient survival rates? Originally published on June 9, 2016 4:47 pm For the roughly 15,000 people who…
The big day. My alarm goes off at 4am, there was no need I was already awake. I don’t feel scared, more of a feeling of nervous anticipation. Same kind of feeling I had before my C sections with my children. I take a shower, as I come out of the bathroom my husband is…
June 10th It’s been a tough week. Have felt increasingly unwell seen at home by a doctor from the local surgery with talk of admitting me to hospital or organising respite care of some form. My own GP was obviously concerned and got in touch…
I’m looking into the subject of cannabis use to try and ascertain what the official position is on whether use of cannabis prior to transplant is acceptable or is grounds for refusing a transplant. In the US, I have not been able to find an authority who decides such things and currently it appears that…
Liver Transplant Inequity For those facing end stage liver disease, attempts will be made to improve the fairness of liver transplant allocation. In an effort to address and improve the coordination of how organs are assigned to patients on the transplant list, the United Network for Organ Sharing (UNOS) held a public hearing in mid-September…
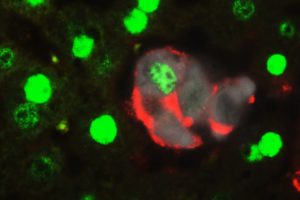
Scientists Find Biological “Switch” That Reverts Mature Liver Cells to Stem Cells June 5, 2014 | by Lisa Winter Photo credit: Picture shows a group of cells transitioning from a mature cell type (green) to a stem cell type (red). White cells are the cells where Hippo is being inactivated. Credit: Dean Yimlamai/Boston Children’s Hospital…
The Wait For A Liver Transplant By LAURAN NEERGAARD 08/20/13 12:36 PM ET EDT WASHINGTON — Where you live can affect your chances of getting a liver transplant, and your risk of dying while waiting. The nation’s transplant network says it’s time to make the system fairer – and it may take a cue from…
Researchers suggest new model for organ allocation Current system relies too heavily on geography, other factors, they say Hub staff report / July 15, 2013 Posted in Voices+Opinion , Health Tagged liver disease , transplants , dorry segev Using the same type of mathematical formulas used to draw political redistricting maps, Johns Hopkins researchers say…