What Is Primary biliary cholangitis?
Primary biliary cholangitis
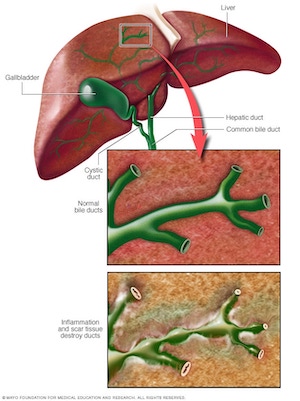
Bile duct damage
Primary biliary cholangitis, previously called primary biliary cirrhosis, is a chronic disease in which the bile ducts in your liver are slowly destroyed. Bile is a fluid made in your liver. It aids with digestion and helps your body get rid of cholesterol, toxins and worn-out red blood cells.
When the bile ducts are damaged, bile can back up in your liver and sometimes lead to irreversible scarring of liver tissue (cirrhosis).
Primary biliary cholangitis is considered an autoimmune disease, which means your body's immune system is mistakenly attacking healthy cells and tissue. Researchers think a combination of genetic and environmental factors triggers the disease. It usually develops slowly. Medication can slow liver damage, especially if treatment begins early.
Symptoms
More than half the people with primary biliary cholangitis do not have any noticeable symptoms when diagnosed. The disease may be diagnosed when blood tests are done for other reasons. Symptoms eventually develop over the next five to 20 years. Those who do have symptoms at diagnosis typically have poorer outcomes.
Common early symptoms include:
Fatigue
Itchy skin
Dry eyes and mouth
Later signs and symptoms may include:
Pain in the upper right abdomen
Swelling of the spleen
Bone, muscle or joint (musculoskeletal) pain
Swollen feet and ankles (edema)
Buildup of fluid in the abdomen due to liver failure (ascites)
Fatty deposits (xanthomas) on the skin around the eyes, eyelids or in the creases of the palms, soles, elbows or knees
Yellowing of the skin and eyes (jaundice)
Darkening of the skin that's not related to sun exposure (hyperpigmentation)
Weak and brittle bones (osteoporosis), which can lead to fractures
High cholesterol
Diarrhea, which may include greasy stools (steatorrhea)
Underactive thyroid (hypothyroidism)
Weight loss
Causes
It's not clear what causes primary biliary cholangitis. Many experts consider it an autoimmune disease in which the body turns against its own cells.
The liver inflammation seen in primary biliary cholangitis starts when certain types of white blood cells called T cells (T lymphocytes) start to collect in the liver. Normally, these immune cells detect and help defend against germs, such as bacteria. But in primary biliary cholangitis, they mistakenly destroy the healthy cells lining the small bile ducts in the liver.
Inflammation in the smallest ducts spreads and eventually damages other cells in the liver. As the cells die, they're replaced by scar tissue (fibrosis) that can lead to cirrhosis. Cirrhosis is scarring of liver tissue that makes it difficult for your liver to work properly.
Risk factors
The following factors may increase your risk of primary biliary cholangitis:
Sex. Most people with primary biliary cholangitis are women.
Age. It's most likely to occur in people 30 to 60 years old.
Genetic factors. You're more likely to get the condition if you have a family member who has or had it.
Geography. It's most common in northern Europe and North America.
Researchers think that genetic factors combined with certain environmental factors trigger primary biliary cholangitis.
These environmental factors may include:
Infections caused by bacteria, fungi or parasites
Smoking
Toxic chemicals
Complications
As liver damage worsens, primary biliary cholangitis can cause serious health problems, including:
Liver scarring (cirrhosis).
Cirrhosis makes it difficult for your liver to work and may lead to liver failure. It indicates the later stage of primary biliary cholangitis. People with primary biliary cholangitis and cirrhosis have a poor prognosis and higher risk of other complications.
Increased pressure in the portal vein (portal hypertension).
Blood from your intestine, spleen and pancreas enters your liver through a large blood vessel called the portal vein. When scar tissue from cirrhosis blocks normal blood flow through your liver, blood backs up. This causes increased pressure inside the vein. Also, because blood doesn't flow normally through your liver, drugs and other toxins aren't filtered properly from your bloodstream.
Enlarged spleen (splenomegaly).
Your spleen can become swollen with white blood cells and platelets because your body no longer filters toxins out of the bloodstream as it should.
Gallstones and bile duct stones. If bile cannot flow through the bile ducts, it may harden into stones, causing pain and infection.
Enlarged veins (varices).
When blood flow through the portal vein is slowed or blocked, blood may back up into other — usually those in your stomach and esophagus. Increased pressure may cause delicate veins to break open and bleed. Bleeding in the upper stomach or esophagus is a life-threatening emergency that requires immediate medical care.
Liver cancer.
Liver scarring (cirrhosis) increases your risk of liver cancer.
Weak bones (osteoporosis).
People with primary biliary cholangitis have an increased risk of weak, brittle bones that may break more easily.
Vitamin deficiencies.
A lack of bile affects your digestive system's ability to absorb fats and the fat-soluble vitamins, A, D, E and K. Because of this, some people with advanced primary biliary may have low levels of these vitamins.
Decreased mental function (hepatic encephalopathy).
Some people with primary biliary cholangitis with liver failure have personality changes and problems with memory and concentration.
Increased risk of other disease. Primary biliary cholangitis is associated with metabolic or immune system disorders, including thyroid problems, limited scleroderma (CREST syndrome) and rheumatoid arthritis.
Prevention
Working together, you and your doctor can help prevent these specific complications:
Increased pressure in the portal vein (portal hypertension). Your doctor is likely to screen and monitor you for portal hypertension and enlarged veins if you have liver disease.
Weak bones (osteoporosis). Exercise most days of the week can help increase your bone density. If you have osteoporosis, your treatment may include calcium and vitamin D supplements.
Vitamin deficiencies.
Your doctor may recommend supplements of vitamins A, D, E and K to improve vitamin levels. Avoid taking herbs or nutritional supplements without talking to your doctor first.
Diagnosis
Your doctor will ask you about your health history and your family's health history, and perform a physical exam.
The following tests and procedures may be used to diagnose primary biliary cholangitis.
Blood tests:
Cholesterol test. More than half the people with primary biliary cholangitis have extreme increases in blood fats (lipids), including total cholesterol level.
Liver tests. These blood tests check the levels of enzymes that may signal liver disease and bile duct injury.
Antibody tests for signs of autoimmune disease. Blood tests may be done to check for anti-mitochondrial antibodies (AMAs). These substances almost never occur in people without the disease, even if they have other liver disorders. Therefore, a positive AMA test is considered a very reliable sign of the disease. However, a small number of people with primary biliary cirrhosis don't have AMAs.
Imaging tests may not be needed. However, they may help your doctor confirm a diagnosis or rule out other conditions with similar signs and symptoms. Imaging tests looking at the liver and bile ducts may include:
Ultrasound. Ultrasound uses high-frequency sound waves to produce images of structures inside your body.
Magnetic resonance cholangiopancreatography (MRCP). This special magnetic resonance imaging (MRI) exam creates detailed images of your organs and bile ducts.
Magnetic resonance elastography (MRE). MRI is combined with sound waves to create a visual map (elastogram) of internal organs. The test is used to detect hardening of your liver that might be a sign of cirrhosis.
Endoscopic retrograde cholangiopancreatography (ERCP). The doctor passes a thin, flexible tube down your throat and injects dye into the area of your small intestine where your bile ducts empty. A tiny camera attached to the end of the tube provides a picture of your bile ducts. This test may be done with or instead of an MRCP. But, it's invasive and may cause complications.
With advances in MRI, it's usually not needed for diagnosis.
If the diagnosis is still uncertain, your doctor may perform a liver biopsy. A small sample of liver tissue is removed through a small incision using a thin needle. It's examined in a laboratory, either to confirm the diagnosis or to determine the extent (stage) of the disease.
Treatment
Treating the disease
There's no cure for primary biliary cholangitis, but medications are available to help slow the progression of the disease and prevent complications. Options include:
Ursodeoxycholic acid (UDCA). This medicine, also known as ursodiol (Actigall, Urso), is commonly used first. It helps move bile through your liver. UDCA doesn't cure primary biliary cholangitis, but it seems to improve liver function and reduce liver scarring. It's less likely to help with itching and fatigue. Side effects may include weight gain, hair loss and diarrhea.
Obeticholic acid (Ocaliva). This is the newest medication approved by the Food and Drug Administration for primary biliary cholangitis. Studies show that when given alone or combined with ursodiol for 12 months it can help improve liver function.
Fibrates (Tricor). Researchers aren't exactly sure how this medicine works to help ease primary biliary cholangitis symptoms. But, when taken with UDCA, it has reduced liver inflammation and itching in some people. More studies are needed to determine long-term benefits.
Other medications. Many other drugs have been used or studied for treating primary biliary cholangitis with mixed results. They include methotrexate (Trexall) and colchicine (Colcrys).
Liver transplant. When medications no longer control primary biliary cholangitis and the liver begins to fail, a liver transplant may help prolong life. A liver transplant replaces your diseased liver with a healthy one from a donor. Liver transplantation is associated with very good long-term outcomes for people with primary biliary cholangitis. However, sometimes the disease comes back several years later in the transplanted liver.
Treating the symptoms
Your doctor may recommend treatments to control the signs and symptoms of primary biliary cholangitis and make you more comfortable.
Treatment for fatigue
Primary biliary cholangitis causes fatigue. But, your daily habits and other health conditions can affect how tired you feel. Researchers are investigating whether a medicine called modafinil (Provigil) may help reduce fatigue in people with primary biliary cholangitis. More research is needed.
Treatment for itching
Antihistamines such as diphenhydramine (Benadryl, others) and loratadine (Claritin, others) are commonly used to reduce itching. They may help with sleep if itching keeps you awake.
Cholestyramine (Questran) is a powder that must be mixed with food or liquids. Though cholestyramine works for most people, the taste is unpleasant.
Rifampin (Rifadin, others) is an antibiotic that may stop itching. Exactly how it does this is unknown. Researchers think it may block the brain's response to itch-inducing chemicals in the blood.
Opioid antagonists such as those containing naloxone (Bunavail, Evzio) and naltrexone (Vivitrol) may help itching related to liver disease. Like rifampin, these drugs seem to reduce the itching sensation by acting on your brain.
Treatment for dry eyes and mouth
Artificial tears and saliva substitutes, available over-the-counter or by prescription, can help ease dry eyes and mouth. Chewing gum or sucking on hard candy also can help you make more saliva and relieve dry mouth.
Lifestyle and home remedies
You may feel better if you take good care of your overall health. Here are some things you can do to improve some primary biliary cholangitis symptoms and, possibly, help prevent certain complications:
Choose reduced-sodium foods. Opt for low-sodium foods or naturally sodium-free foods, since sodium contributes to tissue swelling and to the buildup of fluid in your abdominal cavity (ascites).
Never eat oysters or other raw shellfish. Such seafood can carry infection-causing bacteria, which can be dangerous for people with liver disease.
Exercise most days of the week. Exercise may reduce your risk of bone loss.
Avoid alcohol. Your liver processes the alcohol you drink, and the added stress can cause liver damage. Generally, people with primary biliary cholangitis should abstain from alcohol.
Check with your doctor before starting new medications or dietary supplements. Because your liver isn't working normally, you'll likely be more sensitive to the effects of over-the-counter and prescription medications, as well as some dietary supplements, so check with your doctor before taking anything new.
Coping and support
Living with a chronic liver disease with no cure can be frustrating. Fatigue alone can have a profound impact on your quality of life. Each person finds ways to cope with the stress of a chronic disease. In time, you'll find what works for you. Here are some ways to get started:
Learn about your condition.
The more you understand about primary biliary cholangitis, the more active you can be in your own care. In addition to talking with your doctor, look for information at your local library and on websites affiliated with reputable organizations such as the American Liver Foundation.
Take time for yourself. Eating well, exercising and getting enough rest can help you feel better.
Try to plan ahead for times when you may need more rest.
Get help. If friends or family want to help, let them. Primary biliary cholangitis can be exhausting, so accept the help if someone wants to do your grocery shopping, wash a load of laundry or cook your dinner. Tell those who offer to help what you need.
Seek support. Strong relationships can help you maintain a positive attitude. If friends or family have a hard time understanding your illness, you may find that a support group can be helpful.
Preparing for your appointment
If you have signs or symptoms that worry you, make an appointment with your doctor. If you're diagnosed with primary biliary cholangitis, you may be referred to a doctor who specializes in disorders of the digestive system (gastroenterologist) or liver diseases (hepatologist).
Because there's often a lot to cover during your appointment, it's a good idea to arrive well-prepared.
What you can do
Be aware of any pre-appointment restrictions. At the time you make the appointment, be sure to ask if there's anything you need to do in advance, such as restrict your diet.
Write down any symptoms you're experiencing, including those that may seem unrelated to the reason for which you scheduled the appointment.
Write down key personal information, including any major stresses or recent life changes.
Make a list of all medications, vitamins and supplements that you're taking.
Ask a family member or friend to come with you. Sometimes it can be difficult to remember all of the information provided to you during an appointment. Someone who accompanies you may remember something that you missed or forgot.
Write down questions to ask your doctor.
Preparing a list of questions can help you make the most of your time with your doctor. For primary biliary cholangitis, some basic questions to ask your doctor include:
What's the most likely cause of my symptoms?
What kinds of tests do I need to confirm the diagnosis? Do these tests require any special preparation?
How severe is the damage to my liver?
What treatments do you recommend for me?
What types of side effects can I expect from treatment?
Are there any other treatment options?
Do I need to change my diet?
Are there brochures or other printed material that I can take with me? What websites do you recommend?
In addition to the questions that you've prepared to ask your doctor, don't hesitate to ask other questions that come to mind during your appointment.
What to expect from your doctor
Your doctor is likely to ask you a number of questions. Being ready to answer them may give you more time to discuss a concern in greater detail. Your doctor may ask:
What symptoms have you been experiencing?
When did you first notice them?
Do you always have symptoms or do they come and go?
How severe are your symptoms?
What, if anything, makes your symptoms better or worse?
Has anyone in your family ever been diagnosed with primary biliary cholangitis?
Do you have any chronic health conditions?
Do you have a history of hepatitis or other liver disease?
Does anyone in your family have liver disease?
How much alcohol do you drink?
What medications are you taking?
Do you take any herbal or natural remedies?