What Is Ascites and Edema?
Ascites and Edema
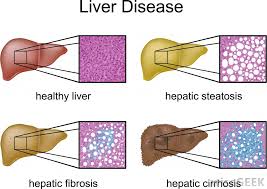
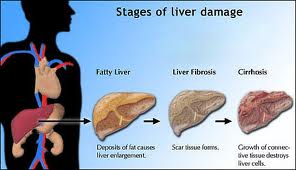
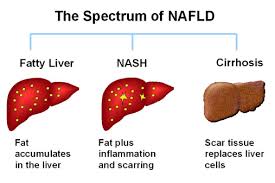
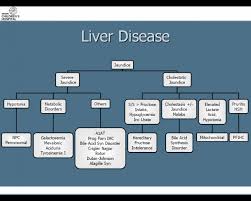
In patients with chronic diseases of the liver, fibrosis (scarring) of the liver often occurs. When the scarring becomes advanced, the condition is called cirrhosis of the liver. Ascites is excessive fluid that accumulates in the abdominal (peritoneal) cavity. It is a complication of cirrhosis and appears as an abdominal bulge.
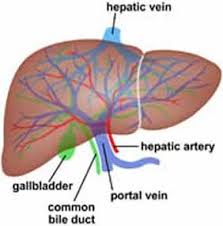
The peritoneum is the inner lining of the abdominal cavity, which also folds over to cover the organs inside the abdomen such as the liver, gallbladder, spleen, pancreas, and intestines.
Ascites develops because of a combination of two factors:
increased pressure in the vein system that carries blood from the stomach, intestines, and spleen to the liver (portal hypertension); and a low level of the protein albumin in the blood (hypoalbuminemia).
Albumin, which is the predominant protein in the blood and which helps maintain blood volume, is reduced in cirrhosis primarily because the damaged liver is not able to produce enough of it.
Other consequences of portal hypertension include dilated veins in the esophagus (varices), prominent veins on the abdomen, and an enlarged spleen. Each of these conditions is due primarily to the increased pressure and accumulation of blood and excess fluid in the abdominal blood vessels.
The fluid of ascites can be removed from the abdominal cavity by using a syringe and a long needle, a procedure called paracentesis. Analysis of the fluid can help differentiate ascites that is caused by cirrhosis from other causes of ascites, such as cancer, tuberculosis, congestive heart failure, and nephrosis.
Sometimes, when ascites does not respond to treatment with diuretics, paracentesis can be used to remove large amounts of the ascitic fluid.
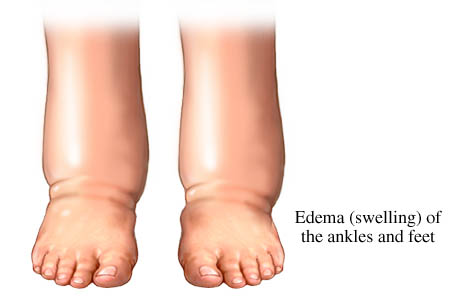
Edema
Peripheral edema, which is usually seen as pitting edema of the legs and feet, also occurs in cirrhosis. The edema is a consequence of the hypoalbuminemia and the kidneys retaining salt and water.
The presence or absence of edema in patients with cirrhosis and ascites is an important consideration in the treatment of the ascites. In patients with ascites without edema, diuretics must be given with extra caution.
Diuresis (induced increased volume of urine by use of diuretics) that is too aggressive or rapid in these patients can lead to a low blood volume (hypovolemia), which can cause kidney and liver failure. In contrast, when patients who have both edema and ascitesundergo diuresis, the edema fluid in the interstitial space serves as somewhat of a buffer against the development of low blood volume.
The excess interstitial fluid moves into the blood vessel spaces to rapidly replenish the depleted blood volume.
Why does edema occur in patients with kidney disease?
Edema forms in patients with kidney disease for two reasons:
a heavy loss of protein in the urine, or
impaired kidney (renal) function.
Heavy loss of protein in the urine
In this situation, the patients have normal or fairly normal kidney function. The heavy loss of protein in the urine (over 3.0 grams per day) with its accompanying edema is termed the nephrotic syndrome. Nephrotic syndrome results in a reduction in the concentration of albumin in the blood (hypoalbuminemia).
Since albumin helps to maintain blood volume in the blood vessels, a reduction of fluid in the blood vessels occurs. The kidneys then register that there is depletion of blood volume and, therefore, attempt to retain salt. Consequently, fluid moves into the interstitial spaces, thereby causing pitting edema.
The treatment of fluid retention in these patients is to reduce the loss of protein into the urine and to restrict salt in the diet. The loss of protein in the urine may be reduced by the use of ACE inhibitors and angiotensin receptor blockers (ARB’s). Both categories of drugs, which ordinarily are used to lower blood pressure, prompt the kidneys to reduce the loss of protein into the urine.
ACE inhibitor drugs include:
enalapril (Vasotec),
quinapril (Accupril),
captopril (Capoten),
benazepril (Lotensin),
trandolapril (Mavik),
lisinopril (Zestril or Prinivil), and
ramipril (Altace).
Angiotensin receptor blockers include:
losartan (Cozaar),
valsartan (Diovan),
candesartan (Atacand), and
irbesartan (Avapro).
Certain kidney diseases may contribute to the loss of protein in the urine and the development of edema. A biopsy of the kidney may be needed to make a diagnosis of the type of kidney disease, so that treatment may be given.
Impaired kidney (renal) function
In this situation, patients who have kidney diseases that impair renal function develop edema because of a limitation in the kidneys’ ability to excrete sodium into the urine. Thus, patients with kidney failure from whatever cause will develop edema if their intake of sodium exceeds the ability of their kidneys to excrete the sodium.
The more advanced the kidney failure, the greater the problem of salt retention is likely to become. The most severe situation is the patient with end-stage kidney failure who requires dialysis therapy. This patient’s salt balance is totally regulated by dialysis, which can remove salt during the treatment.
Dialysis is a method of cleansing the body of the impurities that accumulate when the kidneys fail. Dialysis is accomplished by circulating the patient’s blood over an artificial membrane (hemodialysis) or by using the patient’s own abdominal cavity (peritoneal membrane) as the cleansing surface. Individuals whose kidney function declines to less than 5% to 10% of normal may require dialysis.
How does venous insufficiency cause edema?
The veins in the legs are responsible for transporting blood up to the veins of the torso, where it is then returned to the heart. The veins of the legs have valves that prevent the backward flow of blood within them. Venous insufficiency is incompetence of the veins that occurs because of dilation, or enlargement, of the veins and dysfunction of their valves. This happens, for example, in patients with varicose veins.
Venous insufficiency leads to a backup of blood and increased pressure in the veins, thereby resulting in edema of the legs and feet. Edema of the legs also can occur with an episode of deep vein thrombophlebitis, which is a blood clot within an inflamed vein. In this situation, the clot in the deep vein blocks the return of blood, and consequently causes increased back-pressure in the leg veins.
Venous insufficiency is a problem that is localized to the legs, ankles, and feet. One leg may be more affected than the other (asymmetrical edema). In contrast, systemic diseases that are associated with fluid retention generally cause the same amount of edema in both legs, and can also cause edema and swelling elsewhere in the body.
The response to therapy with diuretic drugs in patients with venous insufficiency tends to be unsatisfactory. This is because the continued pooling of fluid in the lower extremities makes it difficult for the diuretics to mobilize the edema fluid. Elevation of the legs periodically during the day and the use of compression stockings may alleviate the edema. Some patients require surgical treatment to relieve chronic edema that is caused by venous insufficiency.
Which diuretics are used to treat edema?
Edema can become a problem in systemic diseases of the heart, liver or kidneys. Diuretic therapy can be initiated, often alleviating the edema. The most potent diuretics are loop diuretics, so-called because they work in the portion of the kidney tubules referred to as the loop of Henle. The kidney tubules are small ducts that regulate salt and water balance, while transporting the forming urine. Clinical loop diuretics available are:
furosemide (Lasix),
torsemide (Demadex), and
butethamine (Bumex).
The doses of these diuretics vary depending upon the clinical circumstances. These drugs can be given orally, although seriously ill patients in the hospital may receive them intravenously for more prompt or effective response. If one of the loop diuretics is not effective alone, it may be combined with an agent that works further down (more distally) in the tubule.
These agents include the thiazide type diuretics, such as hydrochlorothiazide (HydroDIURIL), or a similar but more potent type of diuretic called metolazone (Zaroxolyn). When diuretics that work at different sites in the kidney are used together, the response often is greater than the combined responses to the individual diuretics (synergistic response).
Some diuretics frequently cause an excessive loss of potassium in the urine, leading to the depletion of body potassium. These drugs include the loop diuretics, the thiazide diuretics, and metolazone. Patients on these diuretics are commonly advised to take potassium supplements and/or to eat foods high in potassium.
High potassium foods include certain fruits such as:
bananas,
orange juice,
tomatoes, and
potatoes.
Patients with impaired kidney function often do not require potassium supplements with diuretics because their damaged kidneys tend to retain potassium. In certain instances, the volume of urine induced by the diuretic can be improved by adding a potassium-sparing diuretic, one that does not cause depletion of potassium.
These diuretics include spironolactone (Aldactone), triamterene (Dyrenium, a component of Dyazide), and amiloride (Midamor). Adding one of these diuretics to the patient’s diuretic regimen may preclude the need for potassium supplements.
Another diuretic that can be used is acetazolamide (Diamox), which counteracts the development of an increased concentration of bicarbonate (too much alkali) in the blood. Increased bicarbonate sometimes occurs in patients receiving other diuretics.
Are diuretics used for other purposes?
Diuretics have several other uses in addition treating edema.
A diuretic may be used as part of the treatment program for patients with hypertension. (High blood pressure may be caused by salt retention, or caused by some antihypertensive medications). In fact, most medications that dilate the blood vessels and reduce blood pressure, except for ACE inhibitors and angiotensin receptor blockers, lead to secondary salt retention by the kidneys.
Thiazide diuretics also have been used to prevent the formation of kidney stones. These drugs reduce the urinary excretion of calcium, which is a component of the kidney stone.
Acetazolamide (Diamox) taken a few days before going to high altitudes, appears to reduce the tendency for people to develop altitude sickness.
Edema At A Glance
Edema is a swelling, usually of the legs, due to the accumulation of excessive fluid in the tissues.
The edema that occurs in diseases of the heart, liver, and kidneys is mainly caused by salt retention, which holds the excess fluid in the body.
In certain liver and kidney diseases, low levels of albumin in the blood can contribute to fluid retention.
Heart failure, cirrhosis of the liver, and a kidney disease called nephrotic syndrome are the most common systemic diseases that cause edema.
Excess fluid that accumulates in the lungs is called pulmonary edema.
Excess fluid that accumulates in the abdominal cavity is called ascites.
Edema of unknown cause occurs primarily in women.
Varicose veins or thrombophlebitis (a blood clot in an inflamed vein) of the deep veins in the legs causes edema that is localized to the legs.
Therapy for edema consists of treating the underlying conditions, restricting salt intake, and often using diuretics (medicines to induce urination).
Similar Articles
- « Previous
- 1
- 2
- 3
- 4
- Next »