Gallstones
Gallstones
Cholelithiasis; Gallbladder attack; Biliary colic; Gallstone attack; Biliary calculus
Last reviewed: August 11, 2011.
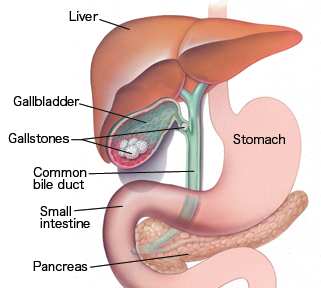
Gallstones are hard, pebble-like deposits that form inside the gallbladder. Gallstones may be as small as a grain of sand or as large as a golf ball.
See also:
Acute cholecystitis
Choledocholithiasis
Causes, incidence, and risk factors
The cause of gallstones varies. There are two main types of gallstones:
Stones made of cholesterol, which are by far the most common type. Cholesterol gallstones have nothing to do with cholesterol levels in the blood.
Stones made of bilirubin, which can occur when red blood cells are being destroyed (hemolysis). This leads to too much bilirubin in the bile. These stones are called pigment stones.
Gallstones are more common in women, Native Americans, Hispanics, and people over age 40. Gallstones may also run in families.
The following also make you more likely to develop gallstones:
Bone marrow or solid organ transplant
Diabetes
Failure of the gallbladder to empty bile properly (this is more likely to happen during pregnancy)
Liver cirrhosis and biliary tract infections (pigmented stones)
Medical conditions that cause the liver to make too much bilirubin, such as chronic hemolytic anemia, including sickle cell anemia
Rapid weight loss from eating a very low-calorie diet, or after bariatric surgery
Receiving nutrition through a vein for a long period of time (intravenous feedings)
Symptoms
Many people with gallstones have never had any symptoms. The gallstones are often found during a routine x-ray, abdominal surgery, or other medical procedure.
However, if a large stone blocks either the cystic duct or common bile duct (called choledocholithiasis), you may have a cramping pain in the middle to right upper abdomen. This is known as biliary colic. The pain goes away if the stone passes into the first part of the small intestine (the duodenum).
Symptoms that may occur include:
Pain in the right upper or middle upper abdomen:
May be constant
May be sharp, cramping, or dull
May spread to the back or below the right shoulder blade
Fever
Yellowing of skin and whites of the eyes (jaundice)
Other symptoms that may occur with this disease include:
Clay-colored stools
Nausea and vomiting
It is important to see a doctor if you have symptoms of gallstones.
Signs and tests
Tests used to detect gallstones or gallbladder inflammation include:
Abdominal ultrasound
Abdominal CT scan
Endoscopic retrograde cholangiopancreatography (ERCP)
Gallbladder radionuclide scan
Endoscopic ultrasound
Magnetic resonance cholangiopancreatography (MRCP)
Percutaneous transhepatic cholangiogram (PTCA)
Your doctor may order the following blood tests:
Bilirubin
Liver function tests
Pancreatic enzymes
Treatment
SURGERY
Some people have gallstones and have never had any symptoms. The gallstones may not be found until an ultrasound is done for another reason. Surgery is usually not needed unless symptoms begin. One exception is in patients who have weight-loss surgery.
In general, patients who have symptoms will need surgery either right away, or after a short period of time.
A technique called laparoscopic cholecystectomy is most commonly used now. This procedure uses smaller surgical cuts, which allow for a faster recovery. Patients are often sent home from the hospital on the same day as surgery, or the next morning.
In the past, open cholecystectomy (gallbladder removal) was the usual procedure for uncomplicated cases. However, this is done less often now.
Endoscopic retrograde cholangiopancreatography (ERCP) and a procedure called a sphincterotomy may be done to find or treat gallstones in the common bile duct.
MEDICATION
Medicines called chenodeoxycholic acids (CDCA) or ursodeoxycholic acid (UDCA, ursodiol) may be given in pill form to dissolve cholesterol gallstones. However, they may take 2 years or longer to work, and the stones may return after treatment ends.
Rarely, chemicals are passed into the gallbladder through a catheter. The chemical rapidly dissolves cholesterol stones. This treatment is not used very often, because it is difficult to perform, the chemicals can be toxic, and the gallstones may return.
LITHOTRIPSY
Electrohydraulic shock wave lithotripsy (ESWL) of the gallbladder has also been used for certain patients who cannot have surgery. Because gallstones often come back in many patients, this treatment is not used very often anymore.
Expectations (prognosis)
Gallstones develop in many people without causing symptoms. The chance of symptoms or complications from gallstones is low. Nearly all patients who have gallbladder surgery do not have their symptoms return (if the symptoms were actually caused by gallstones).
Complications
Blockage of the cystic duct or common bile duct by gallstones may cause the following problems:
Acute cholecystitis
Cholangitis
Cholecystitis – chronic
Choledocholithiasis
Pancreatitis
Calling your health care provider
Call for an appointment with your health care provider if you have:
Pain in the upper part of your abdomen
Yellowing of the skin or whites of the eyes
Prevention
In most people, gallstones cannot be prevented. In people who are obese, avoiding rapid weight loss could prevent gallstones.
References
Siddiqui T. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis: a meta-analysis of randomized clinical trials. Am J Surg. 2008;195(1):40-47. PubMed
Chari RS, Shah SA. Biliary system. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL. Sabiston Textbook of Surgery. 18th ed. St. Louis, Mo: WB Saunders; 2007:chap. 54.
Wang DQH, Afdhal NH. Gallstone disease. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger & Fordtran’s Gastrointestinal and Liver Disease. 9th ed. Philadelphia, Pa: Saunders Elsevier; 2010:chap 65.
Glasgow RE, Mulvihill SJ. Treatment of gallstone disease. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger & Fordtran’s Gastrointestinal and Liver Disease. 9th ed. Philadelphia, Pa: Saunders Elsevier; 2010:chap 66.
Review Date: 8/11/2011.
Reviewed by: Linda J. Vorvick, MD, Medical Director, MEDEX Northwest Division of Physician Assistant Studies, University of Washington, School of Medicine; and George F. Longstreth, MD, Department of Gastroenterology, Kaiser Permanente Medical Care Program, San Diego, California. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M., Inc.