So you think you have cirrhosis – What happens next??
What happens next??
A question asked by most people who initially get diagnosed with this disease is ‘Ok, so what happens next???’
Here are some answers, this is a good primer on what to do next and what to expect.
Treatment Overview
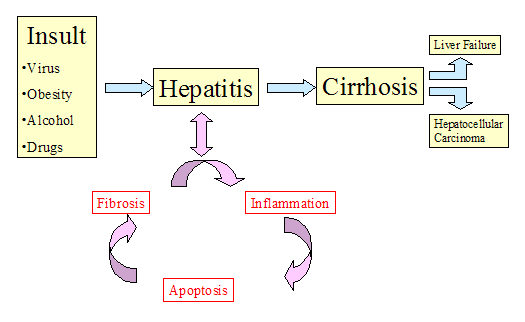
Cirrhosis is a potentially life-threatening condition that occurs when inflammation and scarring damage the liver. No treatment will cure cirrhosis or repair scarring in the liver that has already occurred. But treatment can sometimes prevent or delay further liver damage. The main components of treatment include:
Treating the cause of cirrhosis, when possible, to prevent further liver damage.
Avoiding substances that may further damage the liver, especially alcohol.
Preventing and treating the symptoms and complications of cirrhosis.
Having a liver transplant if your liver damage becomes severe, as long as you are a suitable candidate for liver transplantation and a liver is available.
Initial treatment
If you have just been diagnosed with cirrhosis, which occurs when inflammation and scarring damage the liver, your doctor will recommend that you:
Stop drinking alcohol. You need to quit completely.
Talk to your doctor about all medicines you take, including nonprescription drugs such as acetaminophen, ibuprofen (Advil or Motrin) and naproxen (Aleve).
Begin following a low-sodium diet if fluid retention is occurring. Reducing your sodium intake can help prevent fluid buildup in your abdomen (ascites) and chest.
Get immunized (if you have not already) against Hepatitis A, B, Influenza and Pneumococcus. Taking these steps may help prevent complications and further damage to your liver and help you control symptoms.
Initial treatment of cirrhosis will also include treatment for any complications that have already developed. You may need medications, surgery, or other treatment, depending on what complications you have.
Ongoing treatment
Cirrhosis is a potentially life-threatening condition that occurs when inflammation and scarring damage the liver. Ongoing treatment for the disease focuses on watching for, trying to prevent, and treating symptoms and complications.
You must continue to:
Avoid all alcohol.
Make sure your doctor knows all of the medicines you are taking, including nonprescription drugs.
Begin or stay on a low-sodium diet if fluid retention begins occurring or continues, to help reduce fluid buildup and its complications.
Depending on what complications develop, you may need medicines, surgeries, or other treatments.
Fluid buildup in the abdomen (ascites) is one of the most common problems for people with cirrhosis and can become life-threatening if it is not controlled. Following a low-sodium diet can help reduce fluid buildup in the abdomen. But you may also need:
Diuretic medicines, such as spironolactone and furosemide, to help eliminate fluid that has built up in the abdomen and other parts of the body. These medicines can help both prevent and treat problems with ascites. Your doctor may prescribe a diuretic for you to take over the long term.
Paracentesis with or without a protein (albumin) infusion. Paracentesis is a procedure in which a needle is inserted through the abdominal wall to remove fluid from the abdominal cavity. It may be used to treat severe ascites that is causing symptoms and is not responding to standard treatment with diuretics and a low-sodium diet.
Antibiotics, such as ciprofloxacin (Cipro) or cefotaxime (Claforan), if you develop a bacterial infection in your abdomen (spontaneous bacterial peritonitis, or SBP) as a result of fluid buildup.
Transjugular intrahepatic portosystemic shunt (TIPS). This procedure can divert fluid from the abdominal cavity and may be used to treat ascites that does not respond to other forms of treatment.
Bleeding from enlarged veins in the digestive tract (variceal bleeding) is another common and potentially life-threatening problem for people with cirrhosis. It is particularly important to avoid aspirin and NSAIDs if you have variceal bleeding or are at high risk for it. You may also need:
Beta-blocker medicines, such as propranolol and nadolol. These medicines decrease the risk of variceal bleeding caused by portal hypertension.
Beta-blockers may help lower the pressure in the portal veins, which can reduce your risk of having a first episode of variceal bleeding. These medicines also may be used to reduce the risk of recurrent bleeding.
Vasoconstrictor medicines. These medicines are used to treat a sudden (acute) episode of variceal bleeding. They reduce blood flow through the portal veins by temporarily narrowing the blood vessels. Somatostatin and octreotide are medicines commonly used in the United States.
Endoscopic variceal banding or sclerotherapy. These techniques may be used to treat and prevent variceal bleeding in the esophagus. In the past, sclerotherapy was the main treatment for a first episode of variceal bleeding, but it is now used mostly in emergency situations. Most doctors now prefer variceal banding because it works as well as sclerotherapy to stop bleeding and has fewer complications.4, 1
Shunts. These procedures redirect the flow of blood through other areas of the body. One type of shunt is atransjugular intrahepatic portosystemic shunt (TIPS). This procedure may be used to treat variceal bleeding that does not respond to other less invasive or less risky forms of treatment.
Balloon tamponade, also called a Sengstaken-Blakemore tube. Insertion of a Sengstaken-Blakemore tube is a temporary treatment that may be done to stop severe variceal bleeding and help stabilize your condition before another therapy is tried or before you can be moved to a facility that can perform treatment. It also may be done if nothing else has worked to stop bleeding. A doctor inserts and inflates a balloon in the stomach. The balloon presses against the enlarged veins to stop bleeding. This treatment is rarely necessary.
Changes in mental function (encephalopathy) may develop when the liver cannot filter poisons from the bloodstream, especially substances produced by bacteria in the large intestine. As these toxins build up in your blood, they can affect your brain function. To prevent or treat encephalopathy, you may need to:
Take lactulose, a medicine that helps prevent the buildup of ammonia and other natural toxins in the large intestine.
Eat a modest amount of protein. Your body needs protein to function well but, if your liver damage is severe, your body may not be able to use protein properly, which can contribute to the buildup of harmful toxins. A registered dietitian can help you learn to eat a healthy diet.
Avoid sedative medicines, such as sleeping pills, antianxiety medicines, and narcotics. These can make symptoms of encephalopathy worse.
Working with your doctor to monitor your condition is also important, especially because symptoms may not start until a problem has become severe. In addition to regular checkups and lab tests with your doctor, you also need periodic screening for enlarged veins (varices) and liver cancer (hepatocellular carcinoma).
The American College of Gastroenterology recommends screening for varices with endoscopy for all people who have cirrhosis. If your initial screening does not find any varices, you can be screened again in 1 to 2 years. If you already have large varices, you may need more frequent screening and treatment with beta-blocker medicines to try to prevent future bleeding episodes. If you have had an episode of variceal bleeding, you may need more frequent screening and beta-blocker medicine, or your doctor may recommend variceal banding to help prevent future bleeding.
Screening for liver cancer should take place every 6 months to 1 year. The usual screening is a combination of alpha-fetoprotein testing and liver ultrasound. Research is continuing to find more precise screening tools. One tool that shows promise for detecting liver cancer is computed tomography (CT).5Magnetic resonance imaging (MRI) may also be useful.
Cirrhosis is usually a progressive condition. Before your condition becomes severe, you may want to talk to your doctor about future treatment possibilities. In particular, you may want to discuss:
Whether you will be a good candidate for a liver transplant if your disease becomes advanced. Talk about what steps you can take now to improve your overall health so that you can increase your chances of being considered a suitable candidate.
What level of medical intervention you want as you approach the end of life. Some people want every possible medical treatment to sustain life. Others prefer measures to maintain comfort without prolonging life. Advanced cirrhosis can affect your brain function, so it makes sense to consider these issues while you are still able to make and communicate decisions.
Treatment if the condition gets worse
Cirrhosis is a potentially life-threatening condition that occurs when inflammation and scarring damage the liver. As cirrhosis and liver damage get worse, you may develop more problems with fluid buildup in the abdomen (ascites), bleeding from enlarged veins in the digestive tract (variceal bleeding), changes in mental function (encephalopathy), and other complications. You may need a combination of medicines, surgeries, and other treatments, depending on the nature and severity of the problems.
Receiving a liver from an organ donor (liver transplantation) is the only treatment that will restore normal liver function and cure portal hypertension. Liver transplantation is usually considered only when liver damage is severe and threatening your life. Most people who receive liver transplants have end-stage cirrhosis and severe complications of portal hypertension.
Liver transplant surgery is very expensive. You may have to wait a long time for a transplant because so few organs are available. Even if a transplant occurs, it may not be successful. With these things in mind, doctors must decide who will benefit most from receiving a liver transplant.
Liver transplantation may be an option if you have end-stage cirrhosis and are a good candidate for the surgery. Good candidates include those who:Liver transplant may not be a good option if you have other serious medical conditions (such as heart or lung conditions) that reduce your chance of surviving surgery or that would reduce your life expectancy even if you received a new liver.
Have not abused alcohol or illegal drugs for the previous 6 months.
Have a good support system of family and friends.
Can stay on a complicated regimen of post-transplant medicines to prevent the body from rejecting the liver.
Palliative care
If your cirrhosis gets worse, you may want to think about palliative care. Palliative care is a kind of care for people who have illnesses that do not go away and often get worse over time. It is different than care to cure your illness, called curative treatment. Palliative care focuses on improving your quality of life—not just in your body, but also in your mind and spirit. Palliative care can be combined with curative care.
Palliative care may help you manage symptoms or side effects from treatment. It could also help you cope with your feelings about living with a long-term illness, make future plans concerning your medical care, or help your family better understand your illness and how to support you.
If you are interested in palliative care, talk to your doctor. He or she may be able to manage your care or refer you to a doctor who specializes in this type of care.
For more information, see the topic Palliative Care.
End-of-life issues
If you have not already made decisions about the issues that may arise at the end of life, consider doing so now. Many people find it helpful and comforting to state their health care choices in writing (with an advance directive such as a living will) while they are still able to make and communicate these decisions. You may also think about who you would choose as your healt