The Pancreas
November 26, 2012
The Pancreas

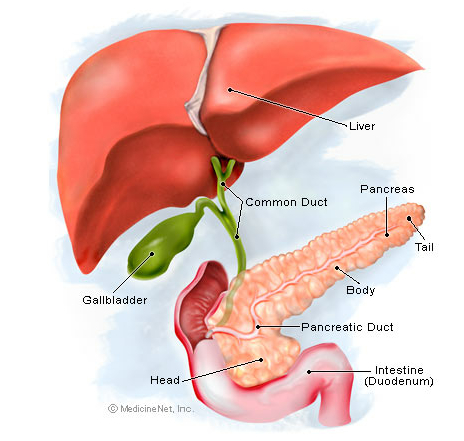
Picture of the Pancreas
Front View of the Pancreas
The pancreas is about 6 inches long and sits across the back of the abdomen, behind the stomach. The head of the pancreas is on the right side of the abdomen and is connected to the duodenum (the first section of the small intestine) through a small tube called the pancreatic duct. The narrow end of the pancreas, called the tail, extends to the left side of the body.
Pancreas Conditions
- Diabetes, type 1: The body’s immune system attacks and destroys the pancreas’ insulin-producing cells. Lifelong insulin injections are required to control blood sugar.
- Diabetes, type 2: The pancreas loses the ability to appropriately produce and release insulin. The body also becomes resistant to insulin, and blood sugar rises.
- Cystic fibrosis: A genetic disorder that affects multiple body systems, usually including the lungs and the pancreas. Digestive problems and diabetes often result.
- Pancreatic cancer: The pancreas has many different types of cells, each of which can give rise to a different type of tumor. The most common type arises from the cells that line the pancreatic duct. Because there are usually few or no early symptoms, pancreatic cancer is often advanced by the time it’s discovered.
- Pancreatitis: The pancreas becomes inflamed and damaged by its own digestive chemicals. Swelling and death of tissue of the pancreas can result. Although alcohol or gallstones can contribute, the cause of most pancreatitis is unknown.
- Pancreatic pseudocyst: After a bout of pancreatitis, a fluid-filled cavity called a pseudocyst can form. Pseudocysts may resolve spontaneously, or they may need surgical drainage.
- Islet cell tumor: The hormone-producing cells of the pancreas multiply abnormally, creating a benign or cancerous tumor. These tumors produce excess amounts of hormones and then release them into the blood. Gastrinomas, glucagonomas, and insulinomas are examples of islet cell tumors.
- Enlarged pancreas: An enlarged pancreas may mean nothing. You may simply have a pancreas that is larger than normal. Or, it can be because of an anatomic abnormality. But other causes of an enlarged pancreas may exist and require treatment.
Pancreas Tests
- Physical examination: By pressing on the center of the belly, a doctor might check for a mass in the pancreas. He or she can also look for other signs of pancreas conditions.
- Computed tomography scan: A CT scanner takes multiple X-rays, and a computer creates detailed images of the pancreas and abdomen. Contrast dye may be injected into your veins to improve the images.
- Magnetic resonance imaging (MRI): Magnetic waves create highly detailed images of the abdomen. Magnetic resonance cholangiopancreatography (MRCP) is an MRI that focuses on the pancreas, liver, and bile system.
- Endoscopic retrograde cholangiopancreatography (ERCP): Using a camera on a flexible tube advanced from the mouth to the intestine, a doctor can access the area of the pancreas head. Tiny surgical tools can be used to diagnose and treat some pancreas conditions.
- Pancreas biopsy: Either using a needle through the skin or a surgical procedure, a small piece of pancreas tissue is removed to look for cancer or other conditions.
- Ultrasound: A probe is placed on the belly, and harmless sound waves create images by reflecting off the pancreas and other organs.
- Amylase and lipase: Blood tests showing elevated levels of these pancreatic enzymes can suggest pancreatitis.
- Sweat chloride test: A painless electric current stimulates the skin to sweat, and the chloride in perspiration is measured. People with cystic fibrosis often have high sweat chloride levels.
- Genetic testing: Many different mutations of a single gene can cause cystic fibrosis. Genetic testing can help identify if an adult is an unaffected carrier or if a child will develop cystic fibrosis.
Pancreas Treatments
- Insulin: Injecting insulin under the skin causes body tissues to absorb glucose, lowering blood sugar. Insulin can be created in a lab or purified from animal sources.
- Pseudocyst drainage: A pseudocyst can be drained by inserting a tube or needle through the skin into the pseudocyst. Alternately, a small tube or stent is placed between either the pseudocyst and the stomach or the small intestine, draining the cyst.
- Pseudocyst surgery: Sometimes, surgery is necessary to remove a pseudocyst. Either laparoscopy (multiple small incisions) or laparotomy (one larger incision) may be needed.
- Pancreatic cancer resection (Whipple procedure): The standard surgery to remove pancreatic cancer. In a Whipple procedure, a surgeon removes the head of the pancreas, the gallbladder, and the first section of the small intestine (the duodenum). Occasionally, a small part of the stomach is also removed.
- Pancreatic enzymes: People with cystic fibrosis often must take oral pancreatic enzymes to replace those that the malfunctioning pancreas doesn’t make.
- Pancreas transplantation: An organ donor’s pancreas is transplanted into someone with diabetes or cystic fibrosis. In some patients, a pancreas transplant cures diabetes.
- Islet cell transplantation: Insulin-producing cells are harvested from an organ donor’s pancreas and transplanted into someone with type 1 diabetes. The still-experimental procedure can potentially cure type 1 diabetes.