Fatty liver disease has gone from unknown to pandemic, but does it mean anything?
Fatty liver disease has gone from unknown to pandemic, but does it mean anything?
By Druin Burch |Posted Friday, Dec. 14, 2012, at 12:51 PM ET
Foie gras.
Foie gras—essentially fatty liver—is delicious. Is it a disease?
Diseases come and diseases go—which, when you think about it, they really shouldn’t. Outside of diseases that have been eradicated, this inconstancy suggests a certain fallibility and fashion running through medicine, a discipline we’d prefer to be a reliable science. Take chlorosis. For hundreds of years doctors understood it perfectly. It afflicted young women, coloring their complexion with an unmistakeable trace of green. Unrequited love was the cause—or, to put it in the physical terms used more often, the lingering and harmful persistence of female virginity. In 1936, chlorosis was officially demolished as a condition.Unsatisfied physical longing as a cause of green-tinged skin disappeared from the medical world.
It’s no surprise to find our ancestors getting things wrong—they were, after all, an ignorant and prejudiced lot. But could it be that our world has not yet reached a stage of mental and cultural perfection? Might we be making similar mistakes, inventing diseases that don’t really exist? And if we are, does it matter?
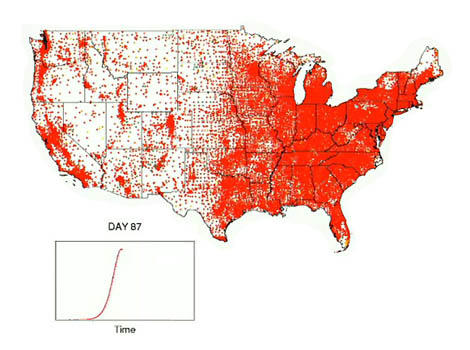
Consider these questions in relation to something which, before 1980, wasn’t described as a disease. You might call it the human version of foie gras. Or, if you felt diseases benefited from being described in Greek (a lingering medical conviction, and one I confess to sharing), you’d name it hepatic steatosis or even steatohepatitis. If you favored plain language, you’d call it fatty liver disease.Whatever name you chose, you’d be referring to a condition which has gone from unknown to pandemic within a few decades, all without any change in human hepatic physiology. Fatty liver disease affects up to a quarter of us . Its harms—a significantly increased risk of death among them—are taken seriously by hepatologists and other doctors. But it may not be a real disease at all.
Contemplate for a moment one of the ethical quirks of the debate about foie gras. Even if you accept that force-feeding geese is cruel, you can still produce foie gras as ethically sound as any meat product. One of the functions of the liver is the storage of energy, and birds that go on long migrations lay down fat in preparation. Slaughter a goose just before it’s expecting to take off across the globe, and you can extract a foie with the gras a gourmand desires. Fatty livers in geese, then, aren’t necessarily a disease—they can be a healthy consequence of the animal storing energy it’s expecting to need.
Something similar happens in humans, with the key problem being that our tendency to lay down calories is out of proportion with our likelihood of using them up. We’re good at storing up fat—padding out our bellies, our bottoms, our livers, and the rest of our generally overfed and under-exercised bodies. We’re evolutionarily adapted for boom and bust, for periods of plenty and periods of want. Faced with a constant supply of food, we eat it. We put on weight and then we put on more. That’s a real challenge, but just possibly I’m not the first to break this news. We know that obesity is unhealthy and that it’s on the rise.It’s something we’re bad at dealing with, both emotionally and practically. We even agonize over it morally. Doctors and society tend to blame the overweight for their condition with a disapproval that we don’t apply, say, to mountaineers who fall and break bones. As medics, we’re also lousy at actually helping. A lot of research money goes into weight-loss drugs, which at best are minimally effective and tend to have nasty side effects. Relatively little goes into figuring out how to engineer societies to eat less and exercise more—and even when it does, we worry how much of that sort of societal engineering we should be doing. The appropriate boundary between invading individual freedom and promoting public health can be pretty unclear.
Those with fatty liver disease won’t know for certain they have the disease without a scan, be it ultrasound or some other modality. Usually fatty liver disease causes no symptoms. Yet those who have it are more likely to suffer heart attacks and strokes, more likely to develop liver cirrhosis, more likely to have high blood pressure and diabetes. Their health is improved from lowering their blood pressure and cholesterol levels, from dieting and exercising, and even (if they’re particularly obese) from having a gastric bypass or similar surgery to help them lose weight. So why isn’t it necessarily a real disease?
The problem comes into focus when you realise these same hazards and recommendations can be invoked for any other manifestation of being overweight. Take fatty elbow disease. As far as I’m aware, I’m the first to describe it, but I think it could take off. It’s associated with being overweight and under active and it carries with it the same range of real risks. Sufferers are often asymptomatic, unaware of their illness, although I admit that it can be picked up without much use of an MRI scanner. Shortly I’ll be writing to the New England Journal of Medicine to expose the problem. I’ll demand action to raise the profile of fatty elbow disease, with programs to screen elbows nationwide and make patients aware of their affliction. I’ll accept lucrative posts advising drug companies and seek out a celebrity patient or two. I’ll attend so many lavish conference dinners I may develop the disease myself.
Yet there’s a problem. When you say that patients are unaware of their condition, you’re suggesting, in a vital way, that maybe they’re not actually patients. The word comes from pathos, meaning one who suffers. These people are not literally dis-eased, at least not until I disturb their ease by pointing out they suffer from FED. (I feel a flush of parental pride contemplating how technical and impressive it sounds as an acronym.) Do I do people a favor by revealing to them their unsuspected diagnosis? I’m not sure I do. Most people are aware that it’s not ideal to be overweight, to have high blood pressure and high cholesterol, to undertake too little physical exercise. Fatty elbow disease gives me another tool to beat them up with, to add to their sense of guilt. Who knows, they may turn out to have fatty liver disease also, and fatty hip disease, too—they could be suffering under the delusion of reasonable health, when all along they’re a walking bag of medical problems. I worry, though, that I’m just dishing out disease labels for my own benefit, not for the good of the people I’m meant to be caring for. For the foreseeable future, the mortality rate for life is expected to remain at around 100 percent. Staying alive as long as possible is great, and worrying about illness is reasonable, but all life is limited and it’s important to enjoy what we’ve got. Health, like beauty, is terrifically subjective.Tell someone who’s feeling fine that they’ve got fatty liver disease, and you’re subtracting from their sense of well-being. Maybe not much, but you’re doing so all the same, and I’m not sure it’s merited. Remember that shady border between intruding on freedom and promoting health? You may have just crossed it.
Fatty liver disease appears to be a manifestation of what could be called—with justification—Modern Life. We eat too much and we do too little, and one of the things that follows is that we put on weight. As a doctor, I know too little about how to help people deal with that. But banal advice doesn’t cut it, nor does piling on the guilt. The existence of chlorosis said something about our ancestors’ ambivalence toward female sexuality. Fatty liver disease, I suspect, comes from our mixed feelings over modern lifestyles and who to blame for them. It’s not good for us to spend too much time eating and sitting and not enough fasting or running around, but is it really a disease? I think we’re unsure and bad at facing up to our uncertainty. Moral ambivalence, more than calories, might be driving our contemporary pandemic of fatty liver disease.