What Is Primary Biliary Cirrhosis?
What Is Primary Biliary Cirrhosis?
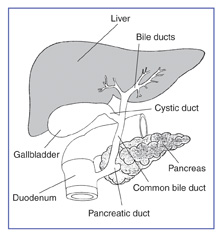
Primary Biliary Cirrhosis (PBC) is a chronic liver disease that slowly destroys the bile ducts within the liver (intrahepatic bile ducts). Liver inflammation over a period of years may cause scarring which leads to cirrhosis. PBC is NOT alcohol or drug related, and it is NOT contagious.
The name “Primary Biliary Cirrhosis” is somewhat deceiving since cirrhosis only occurs in the last stage of the disease (stage 4) after many years of inflammation. With early diagnosis and proper medications, most with PBC will never reach the cirrhosis stage of PBC.
PBC is also called “Chronic Nonsuppurative Destructive Cholangitis” and “Primary Autoimmune Cholangitis.” However, these alternative terms are not widely accepted and therefore not in use.
Definition from New American Medical Dictionary:
Primary: First in order of development, most important, arising spontaneously.
Biliary: Relating to or affecting the bile duct system or bile.
Cirrhosis: An inflammatory disease of the liver associated with the replacement of liver cells by fibrous tissue. Passage of blood through the liver may eventually be obstructed by the cirrhosis.
The cause of PBC is still unknown, but it is not alcohol or drug induced. Current studies suggest it may involve autoimmunity, infection, or genetic predisposition, and does seem to appear more often in certain families. Women are affected 10 times more than men, and PBC is usually diagnosed in patients between the ages of 35 to 60 years.
Those with PBC usually look extremely healthy, and many are 10 to 30 pounds overweight. The slight bronze pigmentation of the skin is often present in the advanced stage of the disease, and makes the individual look tanned. The outward appearances doesn’t tell the story of what is going on inside their bodies. Even on the transplant list stage, many with PBC look healthy. A person with PBC commonly hears comments such as “you look so healthy or you don’t look sick.”
Upon diagnosis, some doctors may suggest their patient start:
Start a reduced sodium diet and or low fat diet. Nutrition
In severely damaged livers, proteins may be restricted.
Drink plenty of water and other fluids such as juice.
Calcuim and Vitamin D. Calcium is the most common mineral in the body and is required for proper functioning of most organs. It is particularly needed in the normal development of the bones and teeth. Osteoporosis is a bone disease where calcium leaves the bones, causing them to weaken, and is commonly associated with PBC.
Avoid or lower intake of alcohol
Lower caffeine intake
Avoid undue stress
Exercise, if possible. Walking is the most common recommendation for exercise.
Stop smoking
The above suggestions have been found to be very helpful in liver disease, but are common sense considered part of healthy living. PBC Menus and meal plans by Norma J. Thiel, RD, Clinical Nutrition Manager Mountainview Hospital.
The number of patients being diagnosed at the asymptomatic stage has risen dramatically over the past few years due to widespread laboratory screening. Typically, the blood lab pattern reveals an elevated alkaline phosphatase level with a normal bilirubin. Bilirubin does not increase until final disease stage. There are four disease stages of PBC.
Medical tests used to confirm PBC:
A liver biopsy helps confirms the diagnosis, but is not a requirement.
Ultrasound exam may be performed to visualize the bile ducts to exclude an obstruction.
Blood lab tests that show liver dysfunction:
Liver function tests
Antimitochondrial antibodies. Positive AMA is found in about 95% of PBC patients.
Serum cholesterol and lipoproteins may be increased.
Haptoglobin & ACE levels may be altered
Diagnostic tests
PBC advances slowly over a period of years. Most patients lead normal lives for years without symptoms, depending on how early diagnosis is made. There is no cure for PBC, but patients are showing good results in slowing the disease progress with URSO 250 , Actigall and methotrexate. With the current medications, it is becoming more common for the PBC patient to live a long life without any complications from PBC, and in some cases actually lowering the disease stage from original diagnosis stage.
PBC is considered an autoimmune disease. Some diagnosed with PBC, may also be diagnosed with one or more other autoimmune diseases. Click for diseases and conditions associated with PBC.
Most patients remain without symptoms for many years, and some may never notice any symptoms. The initial symptoms vary among PBC patients, and the varying symptoms can sometimes make it difficult for doctors to actually diagnose PBC. The varying symptoms may be do to the individual, autoimmune nature or other diseases associated with PBC. Symptoms may be present in any combination and include any of the following:
Fatigue may be the first symptom the patient notices, causing him or her to visit their doctor. The fatigue associated with PBC appears to be totally different from any other sort of fatigue. In early stages, many patients have commented they could sleep for hours. While some in the later stages say sleeping becomes more difficult.
At this time, there is little research into the cause and treatment of the liver disease fatigue. It is usually not due to depression, and some researchers believe it is an abnormality of the axis between the pituitary and the adrenal glands.
Support and understanding from family members, friends and the doctor is very important, making it somewhat bearable.
Intense and unrelenting itching of the skin.
Gradual darkening (hyperpigmentation) or changes in skin texture, and various skin rashes.
Small yellow or white bumps (xanthomas) under the skin, or around the eyes.
Dry Eye Syndrome
Dry mouth, sometimes referred to as cotton mouth.
Thyroid problems
Arthritic aches and pains in bones, muscles and joints are common. In some, the pains can be severe and debilitating. Some even report severe pain just touching leg, feet and hip bones, but this is NOT common.
Over the years, as the PBC progresses, other symptoms may appear.
These symptoms may include any of the following:
Osteoporosis or other metabolic bone disease. See osteoporosis exercises.
Enlarged abdomen from fluid accumulation.
Easy bruising or bleeding
Jaundice (yellowing of the skin and eyes)
Increased bilirubin
Internal bleeding in upper stomach and esophagus, that may be caused by varcies.
Hepatic encephalopathy causing personality changes: dulling of mental functions, neglect of personal appearance, forgetfulness and trouble concentrating, changes in sleeping habits, confusion, breath odor and muscle stiffness. Encephalopathy occurs in final stage of PBC.
Hypersplenism, enlarged spleen
Fever, nausea and vomiting
Reflux and stomach ulcers
Weight increase or decrease
Swelling of the hands, legs and ankles. See edema and ascites
Sexual problems (impotence in men, absence of periods in women, lack of desire.)
Trembling hands
Difficulty in sleeping and changes in sleeping habits. Some PBC patients have noted that itching intensifies when they lay down to sleep, and those who have liver pain say it is more severe in a sleeping position.
Hepatorenal syndrome, progressive deterioration of kidney function leading to kidney failure in a person with liver failure.
Hepatopulmonary syndrome, associated with difficulty with breathing.
Liver cancer (hepatocellular carcinoma)
Abdominal pain or pressure in the liver area. (Yes it’s real)
As the PBC progresses, some patients require vitamin A, vitamin D, vitamin E and vitamin K replacement therapy to add back fat-soluble vitamins which are lost in fatty stools. A calcium supplement may be prescribed to help prevent osteomalacia and osteoporosis.
When medical treatments, such as URSO 250 & URSO Forte, Actigall and methotrexate, no longer control the disease, the patient should be evaluated for a liver transplant. The end stage of PBC is liver failure. Many signs indicate liver failure: increased bilirubin, jaundice, fluid accumulation or ascites, malnutrition, gastrointestinal bleeding, intractable itching, bone fractures and hepatic coma. Transplant is recommended before most of these symptoms occur. Recent studies suggest that about 30% of those diagnosed with PBC will require a transplant. The transplant outcome for PBC patients is excellent.
As with any other chronic illness, support and understanding is very important in helping the PBC patient cope with day to day living.