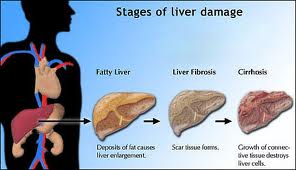
Fibrosis Progression to Cirrhosis
Fibrosis and Cirrhosis
Cirrhosis is a late stage of hepatic fibrosis that has resulted in widespread distortion of normal hepatic architecture. Cirrhosis is characterized by regenerative nodules surrounded by dense fibrotic tissue. Symptoms may not develop for years and are often nonspecific (eg, anorexia, fatigue, weight loss).
Late manifestations include portal hypertension, ascites, and, when decompensation occurs, liver failure. Diagnosis often requires liver biopsy. Cirrhosis is usually considered irreversible. Treatment is supportive.
Cirrhosis is a leading cause of death worldwide. The causes of cirrhosis are the same as those of fibrosis (see Table 1: Fibrosis and Cirrhosis: Disorders and Drugs that Can Cause Hepatic Fibrosis). In developed countries, most cases result from chronic alcohol abuse or chronic hepatitis C. In parts of Asia and Africa, cirrhosis often results from chronic hepatitis B. Cirrhosis of unknown etiology (cryptogenic cirrhosis) is becoming less common as many specific causes (eg, chronic hepatitis C, steatohepatitis) are identified.
Injury to the bile ducts also can result in cirrhosis, such as mechanical bile duct obstruction, primary biliary cirrhosis (see Fibrosis and Cirrhosis: Primary Biliary Cirrhosis (PBC)), and primary sclerosing cholangitis (see Gallbladder and Bile Duct Disorders: Sclerosing Cholangitis).
Pathophysiology
Two primary ingredients exist: hepatic fibrosis and regenerating liver cells. In response to injury and loss, growth regulators induce hepatocellular hyperplasia (producing regenerating nodules) and arterial growth (angiogenesis). Among the growth regulators are cytokines and hepatic growth factors (eg, epithelial growth factor, hepatocyte growth factor, transforming growth factor-α, tumor necrosis factor). Insulin, glucagon, and patterns of intrahepatic blood flow determine how and where nodules develop.
Angiogenesis produces new vessels within the fibrous sheath that surrounds nodules. These “bridges” connect the hepatic artery and portal vein to hepatic venules, restoring the intrahepatic circulatory pathways. Such interconnecting vessels provide relatively low-volume, high-pressure venous drainage that cannot accommodate as much blood volume as normal. As a result, portal vein pressure increases. Such distortions in blood flow contribute to portal hypertension, which increases because the regenerating nodules compress hepatic venules.
The progression rate from fibrosis to cirrhosis and the morphology of cirrhosis vary from person to person. Presumably, the reason for such variation is the extent of exposure to the injurious stimulus and the individual’s response.
Complications:
Portal hypertension (see Approach to the Patient with Liver Disease: Portal Hypertension) is the most common serious complication in the form of GI bleeding from esophageal, gastric, or rectal varices or portal hypertensive gastropathy. Portal hypertension can be massive. Cirrhosis can cause other cardiovascular complications. Vasodilation and intrapulmonary right-to-left shunting and ventilation/perfusion mismatch can result in hypoxia (hepatopulmonary syndrome). A cardiac myopathy can also accompany cirrhosis.
Ascites can develop, with a risk of spontaneous bacterial peritonitis. Splenic congestion with hypersplenism may occur, resulting in splenomegaly and consequent cytopenia. This includes platelet sequestration.
Progressive loss of hepatic architecture impairs function, leading to hepatic insufficiency, manifest by coagulopathy, renal failure (hepatorenal syndrome—see Approach to the Patient with Liver Disease: Renal and Electrolyte Abnormalities), and hepatic encephalopathy. Hepatocytes secrete less bile, contributing to cholestasis and jaundice.
Less bile in the intestine causes malabsorption of dietary fat (triglycerides) and fat-soluble vitamins. Malabsorption of vitamin D may contribute to osteoporosis. Undernutrition is common. It may result from anorexia with reduced food intake or, in patients with alcoholic liver disease, from malabsorption due to pancreatic insufficiency.
Blood disorders are common. Anemia results from hypersplenism, chronic GI bleeding, folate deficiency (particularly in patients with alcoholism), and hemolysis. Clotting may be impaired because of either a coagulopathy or thrombocytopenia. Coagulopathy results from impaired hepatic synthesis of the factors necessary for clotting, malabsorption of vitamin K due to impaired bile secretion into the duodenum, or both.
Thrombocytopenia may be caused by hypersplenism (platelet sequestration), and/or alcohol excess (directly inhibiting the bone marrow). Pancytopenia also occurs with alcoholism.
Hepatocellular carcinoma frequently complicates cirrhosis, particularly cirrhosis resulting from chronic hepatitis B and C viruses, hemochromatosis, alcohol-related liver disease, α1antitrypsin deficiency, and glycogen storage disease.
Histopathology:
Cirrhosis is characterized by regenerating nodules and fibrosis. Incompletely formed liver nodules, nodules without fibrosis (nodular regenerative hyperplasia), and congenital hepatic fibrosis (ie, widespread fibrosis without regenerating nodules) are not true cirrhosis.
Cirrhosis can be micronodular or macronodular. Micronodular cirrhosis is characterized by uniformly small nodules (< 3 mm in diameter) and thick regular bands of connective tissue. Typically, nodules lack lobular organization; terminal (central) hepatic venules and portal triads are distorted.
With time, macronodular cirrhosis often develops. The nodules vary in size (3 mm to 5 cm in diameter) and have some rather normal lobular organization of portal triads and terminal hepatic venules. Broad fibrous bands of varying thickness surround the large nodules. Collapse of the normal hepatic architecture is suggested by the concentration of portal triads within the fibrous scars.
Mixed cirrhosis (incomplete septal cirrhosis) combines elements of micronodular and macronodular cirrhosis. Differentiation between these morphologic types of cirrhosis has limited clinical value.
Symptoms and Signs
Cirrhosis may be asymptomatic for years. One third of patients never develop symptoms. Often, the first symptoms are nonspecific eg, generalized fatigue (due to cytokine release), anorexia, malaise, and weight loss (see Table 2: Fibrosis and Cirrhosis: Common Symptoms and Signs Due to Complications of Cirrhosis). The liver is typically palpable and firm, with a blunt edge, but is sometimes small and difficult to palpate. Nodules usually are not palpable.
Clinical signs that suggest a chronic liver disorder or chronic alcohol use but are not specific for cirrhosis include muscle wasting, palmar erythema, parotid gland enlargement, white nails, clubbing, Dupuytren’s contracture, spider angiomas (< 10 may be normal), gynecomastia, axillary hair loss, testicular atrophy, and peripheral neuropathy.
Once complications of cirrhosis develop, decompensation inexorably ensues.
Diagnosis
General approach: Cirrhosis is suspected in patients with manifestations of any of its complications (see Table 2: Fibrosis and Cirrhosis: Common Symptoms and Signs Due to Complications of Cirrhosis), particularly portal hypertension or ascites. Early cirrhosis should be considered in patients with nonspecific symptoms or characteristic laboratory abnormalities detected incidentally during laboratory testing, particularly in patients who have a disorder or take a drug that might cause fibrosis.
Testing seeks to detect cirrhosis and any complications and determine its cause.
Laboratory tests:
Diagnostic testing begins with liver function tests, coagulation tests, CBC, and serologic tests for viral causes (eg, hepatitis B and C). Laboratory tests alone may increase suspicion for cirrhosis but cannot confirm or exclude it. Liver biopsy becomes necessary if a clear diagnosis would lead to better management and outcome.
Test results may be normal or may detect nonspecific abnormalities due to complications of cirrhosis or alcoholism. ALT and AST levels are often modestly elevated. Alkaline phosphatase and γ-glutamyl transpeptidase (GGT) are often normal; elevated levels indicate cholestasis or biliary obstruction. Bilirubin is usually normal but increases when cirrhosis progresses, particularly in primary biliary cirrhosis (see below).
Decreased serum albumin and a prolonged PT directly reflect impaired hepatic synthesis—usually an end-stage event. Albumin can also be low when nutrition is poor. Serum globulin increases in cirrhosis and in most liver disorders with an inflammatory component. Anemia is common and usually normocytic with a high RBC distribution width. Anemia is often multifactorial: microcytic from chronic GI bleeding; macrocytic from folate nutritional deficiency or hemolysis (especially in alcohol abuse) and hypersplenism.
CBC may also detect leucopenia, thrombocytopenia, or pancytopenia.
Diagnostic imaging:
Imaging tests are not highly sensitive or specific for the diagnosis of cirrhosis by themselves, but they can often detect its complications. In advanced cirrhosis, ultrasonography shows a small, nodular liver. Ultrasonography also detects portal hypertension and ascites.
CT also can detect a nodular texture, but it has no advantage over ultrasonography. Radionuclide liver scans using technetium-99m sulfur colloid may show irregular liver uptake and increased spleen and bone marrow uptake. MRI is more expensive than other imaging tests and has little advantage.
Identification of the cause:
Determining the specific cause of cirrhosis requires key clinical information from the history and findings and selective testing. Alcohol is the likely cause in patients with a documented history of alcoholism and clinical findings such as gynecomastia, spider angiomas (telangiectasia), testicular atrophy, plus laboratory confirmation of liver damage (AST elevated more than ALT) and liver enzyme induction (a greatly increased GGT). Fever, tender hepatomegaly and jaundice suggest the presence of alcoholic hepatitis.
Detecting hepatitis B surface antigen (HBsAg) and IgG antibodies to hepatitis B (IgG anti-HBc) confirms chronic hepatitis B. Identifying serum antibody to hepatitis C (anti-HCV) and HCV-RNA points to hepatitis C.
If common causes such as alcohol or viral hepatitis are not confirmed, other less common causes are sought:
Liver biopsy:
If clinical criteria and noninvasive testing are inconclusive, liver biopsy is usually done. Its sensitivity approaches 100%. Nonalcoholic steatohepatitis (NASH), often associated with obesity, diabetes, or the metabolic syndrome, may be evident on ultrasound scans but requires liver biopsy for confirmation. In obvious cases of cirrhosis with a marked coagulopathy, portal hypertension, ascites, and liver failure, biopsy is not required when management would not change.
Monitoring:
Patients with cirrhosis, particularly if due to chronic viral hepatitis B or C or hemochromatosis, should be screened for hepatocellular carcinoma (eg, measuring α-fetoprotein levels and ultrasonography every 6 to 12 mo—see Liver Masses and Granulomas: Screening).
Prognosis
Prognosis is often unpredictable. It depends on factors such as etiology, severity, presence of complications, comorbid conditions, host factors, and effectiveness of therapy. Patients who continue to drink alcohol, even small amounts, have a very poor prognosis. The Child-Turcotte-Pugh scoring system uses clinical and laboratory information to stratify disease severity, surgical risk, and overall prognosis.