What is a Transjugular Intrahepatic Portosystemic Shunt (TIPS)?
 What is a TIPS?
What is a TIPS?
A transjugular intrahepatic portosystemic shunt (TIPS) is a small, tubular metal device commonly called a stent that is placed in veins in the middle of the liver to improve blood flow to and from the organ.
In a TIPS procedure, interventional radiologists use image guidance to make a tunnel through the liver to connect the portal vein (the vein that carries blood from the digestive organs to the liver) to one of the hepatic veins (three veins that carry blood away from the liver). A stent is then placed in this tunnel to keep the pathway open.
Patients who typically need a TIPS have portal hypertension, increased pressure in the portal vein. This pressure causes blood to flow backward from the liver into the veins of the stomach, lower esophagus, and intestines, causing enlarged vessels, bleeding and the accumulation of fluid in the chest or abdomen.
What are some common uses of the procedure?
A TIPS is used to treat the complications of portal hypertension, including:variceal bleeding, bleeding from any of the veins that normally drain the stomach, esophagus, or intestines into the liver.
portal gastropathy, an engorgement of the veins in the wall of the stomach, which can cause severe bleeding.
severe ascites (the accumulation of high-protein fluid in the abdomen) and/or hydrothorax (in the chest).
Budd-Chiari syndrome, a blockage in one or more veins that carry blood from the liver back to the heart.
How should I prepare?
You should report to your doctor all medications that you are taking, including herbal supplements, and if you have any allergies, especially to local anesthetic medications, general anesthesia or to contrast materials (also known as “dye” or “x-ray dye”).
Your physician may advise you to stop taking aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs) or a blood thinner for a specified period of time before your procedure.
Women should always inform their physician or x-ray technologist if there is any possibility that they are pregnant. Many imaging tests are not performed during pregnancy so as not to expose the fetus to radiation. If an x-ray is necessary, precautions will be taken to minimize radiation exposure to the baby. See the Safety page for more information about pregnancy and x-rays.
You may be instructed not to eat or drink anything after midnight before your procedure. Your doctor will tell you which medications you may take in the morning.
You may drink clear liquids on the day of your procedure.
You should plan to stay overnight at the hospital for one or more days.
You will be given a gown to wear during the procedure.
What does the equipment look like?
In this procedure, x-ray or ultrasound equipment, a stent, and a balloon-tipped catheter are used.
The equipment typically used for this examination consists of a radiographic table, an x-ray tube and a television-like monitor that is located in the examining room or in a nearby room. When used for viewing images in real time (called fluoroscopy), the image intensifier (which converts x-rays into a video image) is suspended over a table on which the patient lies.
When used for taking still pictures, the image is captured either electronically or on film.
Ultrasound scanners consist of a console containing a computer and electronics, a video display screen and a transducer that is used to scan the body and blood vessels. The transducer is a small hand-held device that resembles a microphone, attached to the scanner by a cord.
The transducer sends out high frequency sound waves into the body and then listens for the returning echoes from the tissues in the body. The principles are similar to sonar used by boats and submarines.
The ultrasound image is immediately visible on a nearby screen that looks much like a computer or television monitor. The image is created based on the amplitude (strength), frequency and time it takes for the sound signal to return from the patient to the transducer.
A catheter is a long, thin plastic tube, about as thick as a strand of spaghetti.
The stent used in this procedure is a small wire mesh tube, often covered with a fabric made of GORE-TEX®.
Other equipment that may be used during the procedure includes an intravenous line (IV) and equipment that monitors your heart beat and blood pressure.
How does the procedure work?
A TIPS reroutes blood flow in the liver and reduces abnormally high blood pressure in the veins of the stomach, esophagus, bowel and liver, as well as bleeding from enlarged veins across the esophagus and stomach.
A TIPS procedure involves creating a pathway through the liver that connects the portal vein (the vein that carries blood from the digestive organs to the liver) to a hepatic vein (one of three veins that carry blood from the liver to the heart).
A stent placed inside this pathway keeps it open and allows blood to flow normally from the portal vein through the liver to the hepatic vein, reducing high blood pressure in the portal vein and bleeding from enlarged veins.
How is the procedure performed?
Image-guided, minimally invasive procedures such as a TIPS are most often performed by a specially trained interventional radiologist in an interventional radiology suite or occasionally in the operating room. Some interventional radiologists prefer performing this procedure while the patient is under general anesthesia, while some prefer conscious sedation for their patient.
You will be positioned on your back.
You will be connected to monitors that track your heart rate, blood pressure and pulse during the procedure.
A nurse or technologist will insert an intravenous (IV) line into a vein in your hand or arm so that sedative medication can be given intravenously. You may also receive general anesthesia.
The area of your body where the catheter is to be inserted will be shaved, sterilized and covered with a surgical drape.
Your physician will numb the area near your right collarbone with a local anesthetic.
A very small nick is made in the skin at the site.
Using ultrasound, the doctor will identify your internal jugular vein, which is situated above your collarbone, and guide a catheter, a long, thin, hollow plastic tube into the vessel.
Using a fluoroscope, the physician will then guide the catheter into the liver and out into one of the hepatic veins. Pressures are measured in the hepatic vein and right heart to confirm the diagnosis of portal hypertension, and also to determine the severity.
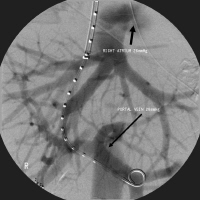
To help plan for the placement of the TIPS stent, a contrast material will be injected in the hepatic vein to outline the portal venous system. Access is then gained from the hepatic vein into the portal system using a TIPS needle (a special long needle extending from the neck into the liver).
A stent is then placed under fluoroscopy extending from the portal vein into the hepatic vein. Once the stent is in the correct position, the balloon is inflated, expanding the stent into place.
The balloon is then deflated and removed along with the catheter. Subsequently, pressures are measured to confirm reduction in portal hypertension. Additional portal venograms are also performed to confirm satisfactory blood flow through the TIPS
Pressure will be applied to stop any bleeding and the opening in the skin is covered with a bandage. No sutures are needed.
You will be admitted to the hospital following your procedure, where you will be closely observed.
This procedure is usually completed in an hour but may take up to several hours depending on the complexity of the condition and vascular anatomy.
What will I experience during and after the procedure?
Devices to monitor your heart rate and blood pressure will be attached to your body.
You will feel a slight pin prick when the needle is inserted into your vein for the intravenous line (IV) and when the local anesthetic is injected.
If you receive a general anesthetic, you will be unconscious for the entire procedure, and you will be monitored by an anesthesiologist.
The intravenous (IV) sedative will make you feel relaxed and sleepy. You may or may not remain awake, depending on how deeply you are sedated.
When the needle is advanced through the liver and the pathway is expanded by the balloon, you may experience discomfort. If you feel pain, you should inform your physician; you may be given extra intravenous medications.
As the contrast material passes through your body, you may get a warm feeling.
After the procedure, you will be monitored closely and your head will be kept elevated for a few hours after you return to your room. Often, symptoms are mild or controlled enough that the procedure can done electively and patients may go home the next day. However, the amount of bleeding that can occur can sometimes be life threatening and those patients are monitored in intensive care beforehand and during recovery.
You should be able to resume your normal activities in seven to 10 days.
Follow-up ultrasounds will be performed frequently after the TIPS procedure to make sure that it remains open and functions properly.
Who interprets the results and how do I get them?
Prior to leaving the hospital, you will have an ultrasound exam to determine the effectiveness of the procedure and placement of the stent.
The interventional radiologist can advise you as to whether the procedure was a technical success when it is completed.
What are the benefits vs. risks?
Benefits
A TIPS is designed to produce the same physiological results as a surgical shunt or bypass, without the risks that accompany open surgery.
TIPS is a minimally invasive procedure that typically has a shorter recovery time than surgery.
Your TIPS should have less of an effect than open surgical bypass on future liver transplantation surgery, because the abdomen has not been entered.
The TIPS is contained entirely inside the diseased liver, and is removed with it during a transplant operation.
Studies have shown that this procedure is successful in reducing variceal bleeding in more than 90 percent of patients.
No surgical incision is needed—only a small nick in the skin that does not have to be stitched closed.
Risks
Any procedure where the skin is penetrated carries a risk of infection. The chance of infection requiring antibiotic treatment appears to be less than one in 1,000.
There is a very slight risk of an allergic reaction to the contrast material used for venograms. Also, renal failure (temporary or permanent) due to contrast material use is a concern, particularly in patients with poor renal function.
Any procedure that involves placement of a catheter inside a blood vessel carries certain risks. These risks include damage to the blood vessel, bruising or bleeding at the puncture site, and infection.
Other possible complications of the procedure include:
fever
muscle stiffness in the neck
bruising on the neck at the point of catheter insertion
delayed stenosis, or narrowing within the stent, which is less common with the current generation of GORE-TEX-lined stents.
Serious complications, reported in fewer than five percent of cases, may include:
occlusion, or complete blockage, of the stent and rapid recurrence of symptoms
infection of the stent or fabric lining
abdominal bleeding that might require a transfusion
laceration of the hepatic artery, which may result in severe liver injury or bleeding that could require a transfusion or urgent intervention
heart arrhythmias or congestive heart failure
radiation injury to the skin is a rare complication (it may happen in complex and lengthy procedures requiring extended fluoroscopy use)
death (rare).
What are the limitations of TIPS?
Patients with more advanced liver disease are at greater risk for worsening liver failure after TIPS. They are also at risk for encephalopathy, which is an alteration of normal brain function that can lead to confusion. This is because toxic substances in the bloodstream are ordinarily filtered out by the liver.
The TIPS may cause too much of these substances to bypass the liver, so a patient who already has encephalopathy because of their liver disease may not be a good candidate for the procedure. Encephalopathy can be treated with certain medications, a special diet or, by revising the stent, but sometimes the stent must be blocked off intentionally to solve the problem.